
Tooth loss can lead to the remodeling of the alveolar ridge, especially the remodeling of the buccal bone wall. This process is usually the reason for the inevitable significant resorption of the alveolar bone within the first three months after tooth loss. The resorption becomes slow after six months and reaches basic stability after one to two years.


Part 1. Physiological Basis and Current Situation of Bone Augmentation Techniques

After tooth extraction, the bundle bone that depends on the existence of the root and periodontal ligament will gradually be resorbed and disappear. During this process, the buccal bone plate mainly composed of bundle bone will show a more obvious decrease in height.
Therefore, when the alveolar bone is insufficient in horizontal and vertical volume, bone reconstruction treatment must be carried out.
In the past 30 years, different techniques and materials have been recommended to reconstruct the defects of the alveolar bone, including autologous, allogeneic or heterogeneous bone grafts.
As early as 1892, the orthopedic surgeon Wolff mentioned that the transplanted bone might heal through osteogenesis, or what he called the osteoblast theory. Wolff pointed out that a large number of osteoblasts and bone cells that survived during the transplantation process were responsible for bone regeneration.
In 1893, a microscopic study by Barth reported that the number of surviving bone cells and osteoblasts was not sufficient to cause bone regeneration. The framework theory was introduced, which achieved bone regeneration through osteoconduction and explained how the mineral part of the graft became the scaffold for the osteoblasts in the recipient area after the biological part died, where the osteoblasts were mainly responsible for bone regeneration.
Modern studies, such as that by Boyne in 1997, proposed the third mode of autologous bone graft regeneration – osteoinduction.
During the process of bone regeneration by osteoinduction, pluripotent stem cells differentiate into bone-forming cells, such as osteoblasts, under the influence of bone morphogenetic proteins, and then produce an osteoid layer on the bone surface, which is subsequently mineralized and transformed into bone cells.
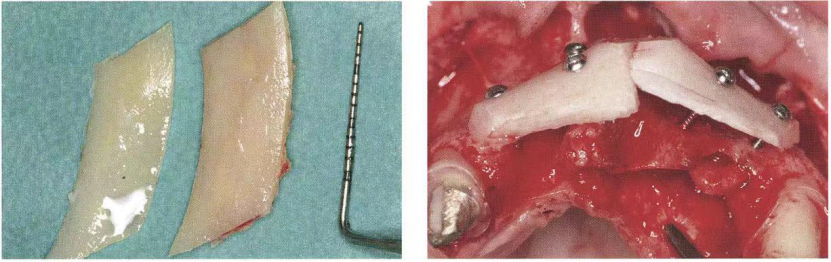
Autologous bone grafts can be taken from multiple intraoral sites, and the most common is to take bone from the buccal bone plate of the mandibular ramus or the median symphysis (chin).
Part 2. Definition and Indications of the Shell Technique
Indications of the “Shell” Technique: For continuous multiple tooth losses accompanied by horizontal and vertical bone defects. For atrophic alveolar ridges with reduced ridge height and a blade-like shape, autologous cortical bone blocks can be fixed on the buccal side of the alveolar ridge, and a scaffold can be created through the shell technique.
Part 3. Operating Steps of the Shell Technique
Application of the “Shell” Technique: A thin bone block is fixed with screws to reconstruct the shape of the alveolar ridge, giving it shape and volume. This thin bone block is fixed with screws at a certain distance from the recipient area rather than in close contact with it, leaving a certain space between the bone block graft and the atrophic alveolar ridge to determine the final shape and thickness of the new alveolar ridge. Then the space between the bone block graft and the recipient area is filled with cancellous bone of the mandible and small cortical bone pieces. This space should be filled with bone particles to prevent the ingrowth of fibroblasts.
After the reconstruction of the alveolar ridge is completed, it is composed of thick internal cancellous bone (cortical bone and cancellous granular bone) and a thin external cortical layer. In the area filled with granular cortical bone and cancellous bone, good vascular distribution can be found, appearing light red, and the external cortical bone is slightly white, which maintains the shape, provides protection and stability for the bone particles. Many blood vessels are observed at the root of the bone graft, providing revascularization and bone regeneration for the transplanted area.


Part 4. Keys to the Success of the Shell Technique

- For continuous multiple tooth losses accompanied by horizontal and vertical bone defects; for atrophic alveolar ridges with reduced ridge height and a blade-like shape, a scaffold can be created by fixing autologous cortical bone blocks on the buccal side of the alveolar ridge to determine the final shape and thickness of the new alveolar ridge. The position of the upper edge of the bone block should be adapted to the position of the planned implant’s buccal bone plate in the future. Meanwhile, the bone block, as an autologous biological membrane, can be used to stabilize the granular bone.
- An open space is created between the alveolar ridge and the bone block to fill with granular autologous bone. These bones are scraped or crushed from the surface of the bone block, having high revascularization and regeneration potentials.
- The key to bone healing is to properly fix the transplanted material so that it cannot be displaced or shaken. If the block autologous bone is not firmly fixed, the risk of infection and resorption is very high. Bone block fixation usually uses titanium nails with an outer diameter of 1.0 – 1.5 mm, and the clamping force of each titanium nail can be as high as 30 kg.

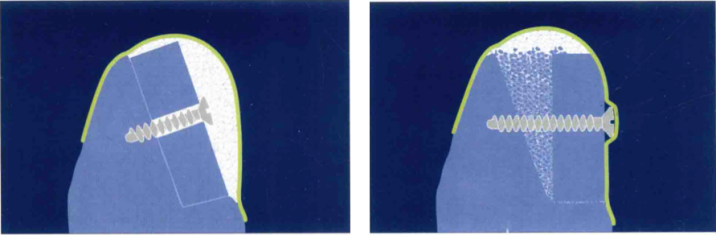
There are lag screws and positioning screws for fixation.
Since the holes in the bone block are slightly wider, the threads of the lag screws do not embed in the bone block.
When the screws are tightened, the bone block is pressed onto the bone surface of the recipient area, and the applied friction makes the bone block stable. If lag screws are not used, usually a hole slightly narrower than the outer diameter of the screw is drilled in the bone block, and then the screw is used to connect the recipient area bone.
The principle of using lag screws to fix the external bone block is to promote healing by establishing close contact between the bone block and the recipient area. The positioning screws can fix the bone block at a certain distance from the bone surface of the recipient area, just like a “Shell”, creating a space that can accommodate granular autologous bone.
References and Books:
Araújo MG, Sukekava F, Wennström JL, et al. Ridge alter- ations following implant placement in fresh extraction sockets: An experimental study in the dog[J]. J Clin Peri- odontol, 2005, 32(6): 645-652.
Fouad Khoury (Germany), translated by Zhang Jian. Soft and Hard Tissue Augmentation in Oral Implantology: Autologous Tissue Transplantation Techniques. Liaoning Science and Technology Press, June 2023.
L. Cordaro (Italy), H. Terheyden (Italy), editors; Su Yucheng, chief translator. Alveolar Ridge Bone Augmentation Procedures in Oral Implantology: Staged Schemes. Liaoning Science and Technology Press, September 2016.




Leave a Reply