There are various tissue organs necessary for maintaining normal physiological activities in the maxillofacial region. Maxillofacial defects will inevitably affect the normal physiological functions of these tissue organs. The development of prosthesis technology has brought acceptable solutions for patients who cannot use autologous or allogeneic tissues for defect repair as the first choice of treatment due to their own conditions, and artificial materials are used for restoration.
Overview
One of the development directions of contemporary maxillofacial defect restoration is the combination of surgical operation and prosthesis technology. Surgical operation is used to create good basic conditions for maxillofacial prosthesis, and then the prosthesis is used to achieve accurate restoration and functional reconstruction. Under the condition that the technical level can be achieved, the best restoration effect is achieved with the least trauma. Compared with other restoration methods, maxillofacial prostheses have the advantages of low cost, short cycle, small trauma, and easy color matching.


The restoration of maxillary defect prostheses is a serialized treatment process. It is divided into three stages: In the first stage, a palatal plate is pre-made before the surgical operation and worn during the operation to isolate food from the wound and facilitate wound recovery. In the second stage, a temporary prosthesis is made 7 – 10 days after the operation to close the oral and nasal cavities and partially restore the functions of chewing, swallowing, and speech. Usually, the final prosthesis restoration begins 3 – 4 months after the wound is stable. Serial prosthesis restoration can maintain the stability of the defect cavity during the whole treatment process, effectively prevent or reduce facial deformities caused by scar contracture during the healing process, and restore or partially restore the swallowing and pronunciation functions of patients.
Digital Application Process
The application of digital technology in the prosthesis treatment process is divided into the following steps:
(1) Digital Model Preparation
The first step is to obtain the three-dimensional data of the patient using digital technology. Patients with maxillary tumors often have complications such as dry mouth and limited mouth opening after radiotherapy and chemotherapy. At this time, using traditional methods to make impressions is a huge challenge for both restorative dentists and patients. To relieve patient discomfort, flap, segment, layer, or individual tray impressions can be taken.


In recent years, the application of digital technology in the field of maxillofacial restoration has increased, and traditional impressions have gradually transformed into digital impressions. Compared with traditional impressions, optical scanning has less irritation to the pharynx, no risk of aspiration, and reduces material waste.
The accuracy of intraoral three-dimensional scanning varies depending on the scanning range, operation experience, etc. However, the accuracy of digital impressions currently basically meets the requirements in fixed denture restoration. Some scholars believe that long dental arch scanning is not suitable for making 5 or more units of fixed partial dentures. Because as the amount of spliced data increases, the accuracy of intraoral scanning decreases. The accuracy of digital impressions in removable restoration still needs to be further improved. The reason is that the alveolar ridge in the edentulous area is smooth and flat, and data splicing is prone to misalignment during intraoral three-dimensional scanning. Although reports on the application of intraoral scanners to scan edentulous jaws are increasing, it is still challenging.
The indirect method is a scanning method that obtains three-dimensional data by scanning traditional impressions or plaster models. Some scholars have concluded through experiments that for full dentition fixed restoration, compared with direct intraoral scanning, the accuracy of obtaining digital models using the indirect method is higher. Some scholars also point out that the indirect method of preparing digital impressions can avoid the influence of tooth reflection, body fluids, etc. on scanning. Compared with intraoral scanning, its resolution and efficiency are higher. For larger-span restorations of 6 or more units, it is recommended to make a physical impression and then scan it outside the mouth.
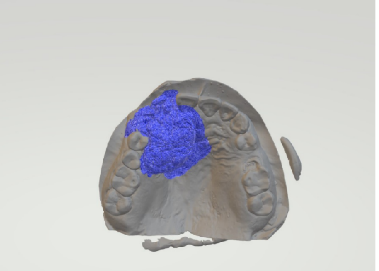
Currently, the digital technology that combines direct and indirect methods is more commonly used in clinical practice. Impressions of the defect cavity and the functional state of the intraoral mucosa are obtained with the assistance of palatal plates or individual trays. According to the characteristic overlap area between the impression scanning data and the intraoral scanning data, registration is carried out. After retaining the respective required parts of the impression and the intraoral scanning data, they are merged and connected to obtain an upper maxillary model with an accurate defect cavity shape.
In addition to digital impression taking, we can also use digital technology for medical imaging reconstruction. In recent years, computed tomography and cone-beam computed tomography have been widely used in the medical field. Some scholars have attempted to reconstruct a three-dimensional model of the maxilla using CBCT data before surgical operation, perform virtual surgical resection on this basis, and then directly design and make a prosthesis, which is worn in the patient’s mouth immediately after the operation. Although this method can prefabricate a prosthesis before the operation and compress and protect the surgical wound in a timely manner after the operation, there may be a difference between the actual surgical resection range and the planned resection range, resulting in the prosthesis not being able to be directly worn.
Some scholars have provided a new solution. Using the characteristic of iodoform gauze being radio-opaque under CBCT, CBCT is taken to reconstruct the defect cavity during the stage of filling the defect cavity with iodoform gauze after the operation, and a temporary prosthesis is designed and made on this basis, which is finally successfully worn in the mouth and has achieved a good sealing effect. This method provides a new solution for reconstructing the maxillary defect model and can make a more accurate prosthesis.

Although CT/CBCT scanning data can reconstruct soft and hard tissue structures, the accuracy of three-dimensional reconstruction of fine tooth structures is not accurate enough to be directly used for making removable or fixed restorations. In addition, when there are metal restorations in the oral cavity, artifacts will be produced, affecting the accuracy of three-dimensional reconstruction of CT/CBCT data. Therefore, combining CT/CBCT with intraoral scanning data has become the choice of most scholars for establishing a jaw defect model.
Research has shown that there is no difference in accuracy between the digital fusion model and the traditional impression, meeting the clinical treatment requirements of maxillary defect restorations.
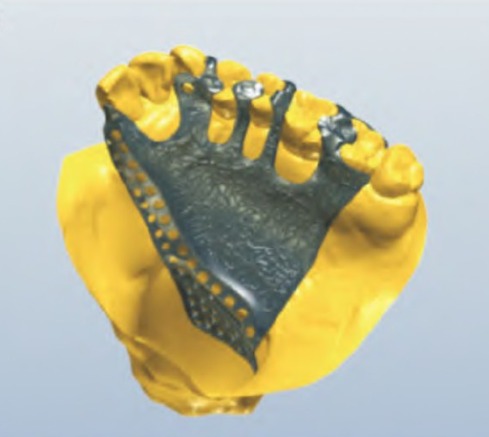
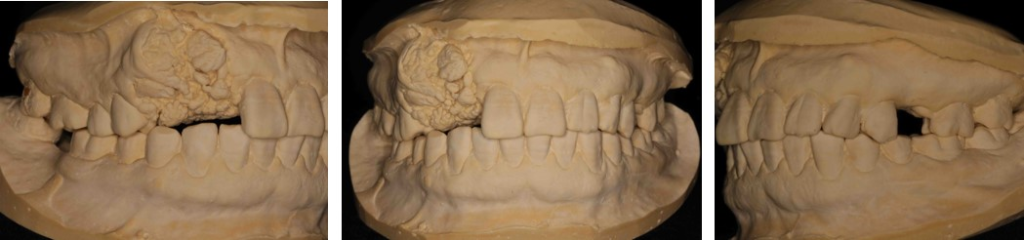
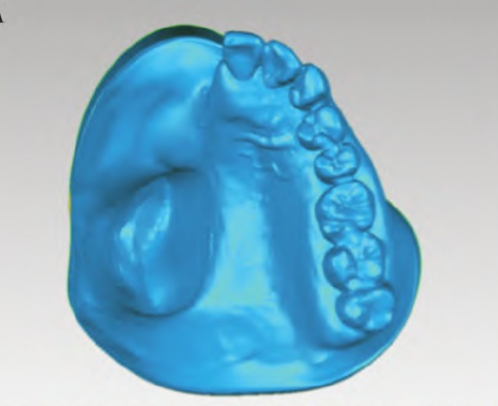
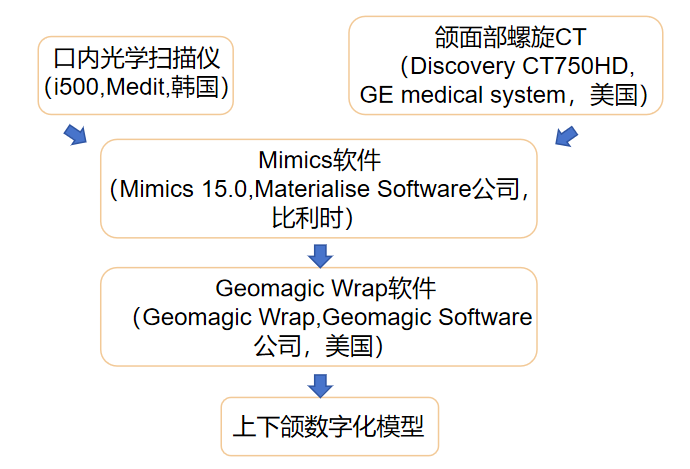
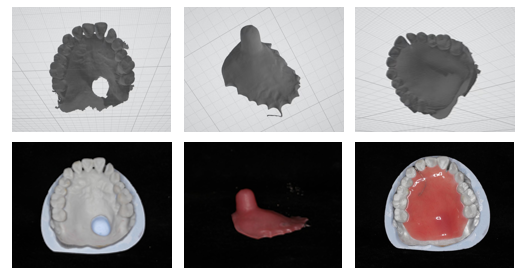
We will understand these processes specifically through a case of making a fully digital maxillary prosthesis. After the patient’s first visit, an intraoral optical scanner is used to scan and obtain the data of the patient’s upper maxillary dentition, defect cavity, palate, lower maxillary dentition, and the occlusion of the remaining teeth. A spiral CT examination of the maxillofacial region is completed. Then, using Mimics software, the soft tissue and bone tissue in the CT are reconstructed and imported into Geomagic Wrap software. The multi-source data of the dentition oral scan data, occlusion data, and spiral CT data are fused to obtain digital models of the upper and lower jaws.
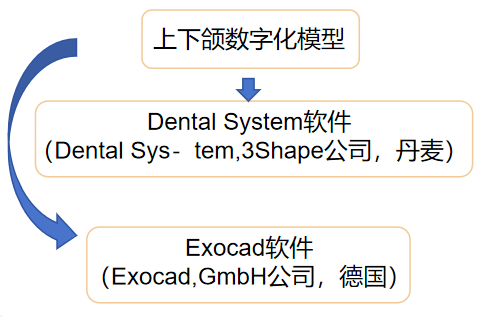
(2) Digital Design
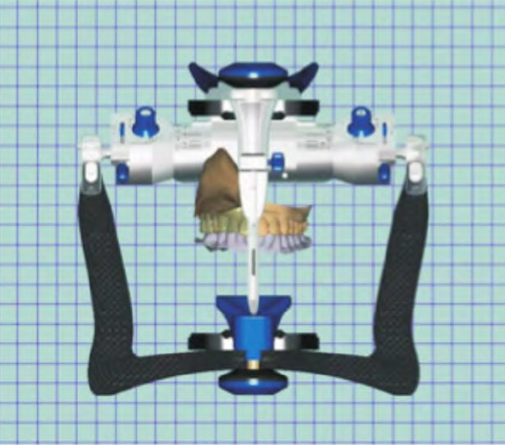
After obtaining the digital model, we can carry out digital design. Using the just obtained data of the upper and lower jaws in the Dental System software, the digital design of the metal bracket is carried out; and the data of the upper and lower jaws and the occlusion data are imported into Exocad software. Using the average value to mount on a virtual frame, the digital arrangement of artificial teeth is completed, and the shape of the obturator corresponding to the shape of the defect cavity is designed. In this way, the digital design of the metal bracket and the obturator is completed.
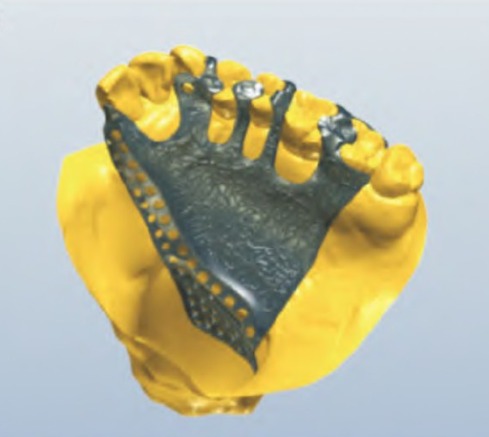
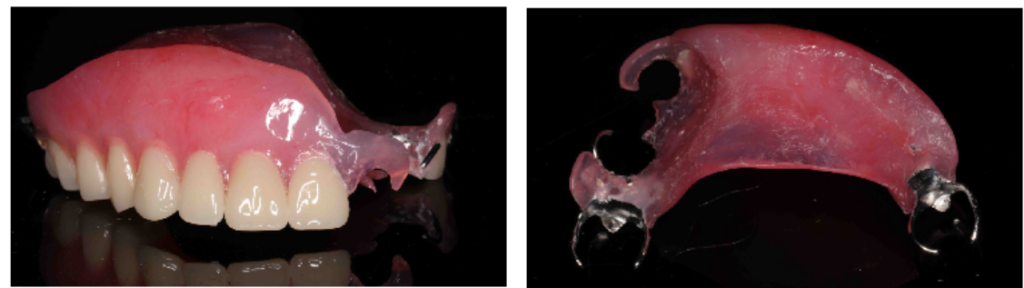
Currently, the main denture design software includes foreign products such as 3Shape, ExoCAD, and domestic removable partial denture software such as IPD, Weishi, etc. When designing restorations at different stages of serial prosthesis restoration, the personalized clinical needs of different restorations need to be considered. When repairing larger range maxillary defects, to reduce the weight of the prosthesis, the obturator part of the prosthesis is generally designed as a hollow structure. Hollow obturators are divided into open and closed types. The closed hollow structure is more commonly used in prosthesis restoration because of its characteristics such as easy cleaning and not easy to retain food. The traditional design and production of the closed hollow structure cannot ensure a consistent thickness and is relatively complex. Using digital software can accurately control the thickness of the hollow obturator part, and the adjustment process is relatively simple. In addition, for the prosthesis design of the bone defect model, to ensure that the bracket has sufficient strength to combine with the base resin in the defect area to form a firm connection, the metal bracket retention network needs to be extended in a certain range in the defect area.
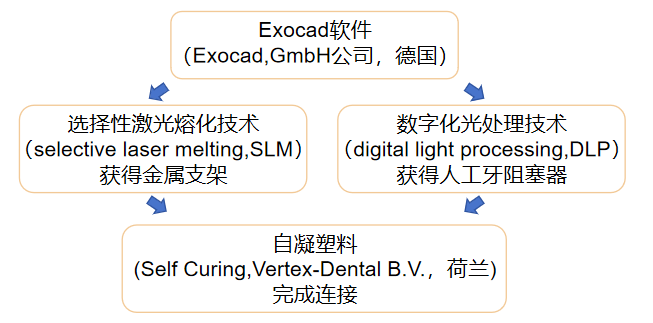
(3) Digital Production
After completing the digital design of the prosthesis, we can then use digital technology to produce it. Digital manufacturing, that is, computer-aided manufacturing, is mainly used to produce resin bases, obturators, and metal brackets for maxillary defect restorations. According of different processing forms, it can be divided into additive manufacturing and subtractive manufacturing. The subtractive technology commonly used in the oral field is numerical control cutting. Its advantage is high processing accuracy, and the repaired object after processing does not require a post-processing process, but the time required for model processing is relatively long, and it cannot cut restorations with a hollow structure.
Additive manufacturing is also called rapid prototyping or 3D printing. It is a layered technology that uses materials to be layered and superimposed to quickly produce three-dimensional objects. Compared with numerical control cutting, 3D printing saves materials and can print prostheses with a hollow design, but the printing cost is relatively high. Currently, there are several methods for additive manufacturing.
Still taking the previous case as an example, after completing the digital design of the prosthesis, a metal bracket is obtained through selective laser melting technology, and an artificial tooth obturator is obtained through digital light processing technology. The two are accurately seated on the model at the same time and then connected with self-curing plastic to obtain the final digital maxillary prosthesis. The patient can complete the initial wearing during the second visit.

Digital Application Efficacy
In the just-mentioned case, the research team compared the traditional prosthesis with the digital prosthesis. One week after wearing the prosthesis, a light-body silicone rubber was used to line the tissue surface of the prosthesis (including the major connector and the defect cavity). After curing, it was removed to ensure that the silicone rubber was not damaged, and the thickness of the light-body silicone rubber was measured as an indicator to evaluate the fit of the prosthesis. The thickness of the silicone rubber was calculated through deviation analysis to reflect the fit of the prosthesis bracket and obturator. The SPSS 23.0 software was used for statistical analysis to calculate the average value and standard deviation of the thickness of the light-body silicone rubber. A paired-sample t-test was used to analyze and compare whether there was a statistical difference in the fit of the prosthesis bracket and obturator between traditional production and digital production. P < 0.05 indicates a statistically significant difference.
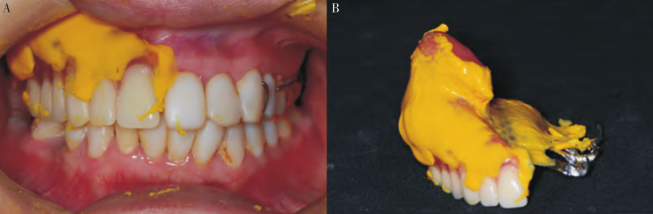
Note: A, Seated and occluded in the mouth; B, The silicone rubber attached to the tissue surface of the prosthesis after being removed
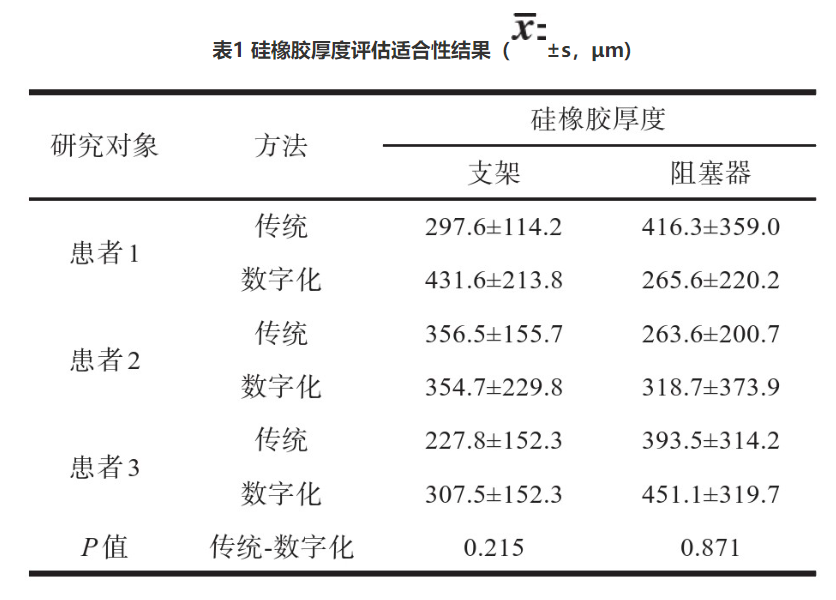
The data of the fit of traditional and digital prostheses for 3 patients are shown in Table 1. The average thickness of the silicone rubber on the tissue surface of the traditional prosthesis bracket is (293.0 卤 64.4) 渭m, and the average thickness of the silicone rubber on the part of the prosthesis defect cavity is (357.8 卤 82.4) 渭m; the average thickness of the silicone rubber on the tissue surface of the digital prosthesis bracket is (364.6 卤 62.6) 渭m, and the average thickness of the silicone rubber on the part of the prosthesis defect cavity is (345.1 卤 95.5) 渭m. The paired t-test shows that there is no statistical difference in the fit of the prosthesis bracket and obturator between the traditional prosthesis and the digital prosthesis.
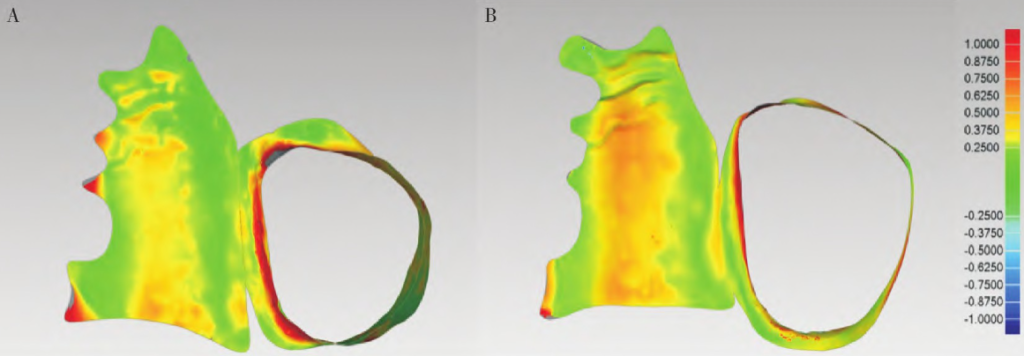
Note: A, Deviation chromatogram of the fit of the traditional prosthesis; B, Deviation chromatogram of the fit of the digital prosthesis
When analyzing the deviation, the maximum critical value is set to 1.0 mm, and the maximum nominal value is 0.25 mm to obtain deviation chromatograms. The traditional prosthesis and the digital prosthesis bracket and obturator all show relatively consistent and good fit, and the deviation chromatograms of the edges of the bracket and obturator and the defect cavity are all green, indicating that the fit of the edges of the bracket and obturator is good.
This research is an exploratory experiment with a small sample size and relatively single clinical application evaluation indicators. However, the research results have preliminarily proved the feasibility of the process and the fit of the digital prosthesis. In subsequent research, a larger sample size randomized controlled trial should be designed, and multiple objective and subjective indicators should be used for comprehensive evaluation.
The ideal restoration state of maxillary defect prosthesis treatment should be: filling the defect, closing the oral-nasal fistula, restoring the physiological functions of chewing, swallowing, and speaking of patients, and improving facial appearance. Some scholars have used digital prostheses to immediately repair 10 patients with maxillary Brown II class defects. After the repair, the speech clarity and swallowing function of the patients have been significantly improved. Currently, digital prostheses have obtained relatively satisfactory clinical results. However, due to the diversity of maxillary defects and the complexity of restoration treatment, most current studies use part of the digital work process, and the clinical application effect of digital technology in prosthesis restoration still needs further research.
Summary and Application Prospect
(1) Limitations
Although the restoration of jaw defect using 3D printed prefabricated prostheses has made great progress compared with traditional prosthesis restoration treatment and has its own personalized advantages compared with free tissue flap repair in surgery, there are still some relatively obvious clinical problems.
(1) There is a certain error in digital scanning
The restoration treatment method of digital prosthesis production avoids the traditional impression method and depends on three-dimensional optical scanning technology to simulate and make models of the patient’s jaw structure and facial shape. However, sometimes it is difficult to accurately capture the morphological information of the edge of the defect area, and there will also be a certain error in reconstructing the defect area through the mirroring principle after collecting facial information digitally, resulting in poor fit between the final prepared prosthesis and the jaw tissue, affecting its retention force.
(2) It is difficult to accurately predict the surgical range
The preoperative surgical simulation and surgical guide design using CAD/CAM technology are almost entirely based on bony tissue, ignoring the information of soft tissues. For patients with primary tumors, the tumor is very likely to invade adjacent surrounding tissues, and the state of soft tissues has an important impact on the surgical resection range. Therefore, once the surgical resection range needs to be changed according to the intraoperative situation, the osteotomy guide plate designed and made based on bony tissue will not be usable, increasing the risk factors of the operation, and blindly expanding the tumor resection range will harm the patient and is not conducive to the post-operative wound healing. Secondly, soft tissues play a role in the fit between the prosthesis and the bony tissue, ignoring the soft tissue structure may lead to poor fit in the end.
(3) The retention is still limited by the amount of remaining tissue
The personalized prosthesis printed by 3D has a much higher accuracy than the traditionally produced prosthesis, and its retention ability is also enhanced. However, it is still limited by the amount of remaining maxillofacial tissue. For patients with large-area maxillary defects, the prosthesis often sinks, and it is still difficult to achieve the ideal retention and restoration effect. Therefore, for patients with large-area jaw defects, free tissue flaps are often used for surgical repair, resulting in a small number of patients available for research on prosthesis restoration, and the existing data is difficult to provide more authoritative and accurate conclusions and guidance.
(4) High requirements for 3D printing bio-materials
In addition to having high requirements for the amount of remaining bone tissue, its long-term restoration effect depends on the 3D printing materials used. 3D printed prefabricated prostheses belong to the manufacture of permanent implants, and they need to use non-degradable biomaterial properties, and currently the supported materials are still very limited, and the situation of color aging after long-term wearing still exists, and the materials used have a certain cytotoxicity to autologous tissue, and the long-term impact on patients after wearing still needs further research.
(5) The application effect evaluation index is not complete
Currently, most domestic studies on the clinical effect of prostheses focus more on the measurement of objective indicators and pay insufficient attention to the subjective feelings of patients. In oral clinical work, it is very important to reasonably analyze the subjective satisfaction of patients because the subjective evaluation of patients can better reflect the overall satisfaction of the treatment and affect the success of the treatment.
(2) Advantages
However, the advantages of digitalization are also equally significant: The digital process of maxillary defect can save clinical operation time, reduce the number of patient visits, and change the traditional diagnosis and treatment process. With the help of CAD/CAM technology and 3D printing, accurate production of entity models, prosthesis brackets, or prostheses can be achieved. Some scholars have reported a case of a patient who had a transverse palatal development disorder due to maxillary hemi-section before puberty and a disordered occlusion relationship of the remaining teeth. Using digital means to determine the fitting path of the restoration, printing the prosthesis bracket was simpler and more accurate than the traditional method. With the development of materials science, 3D printing materials are also being updated continuously. In recent years, PEEK materials have been increasingly used in restoration due to their excellent mechanical properties, chemical stability, and biological safety.
(3) Application Prospect
Combined with the above views, future digital prostheses need to focus on improving the existing deficiencies.
(1) Focus on improving the retention force of prostheses. For example, by designing a hollow prosthesis to reduce the weight of the prosthesis, designing a titanium bracket to provide support and retention, etc.;
(2) Compensate for certain errors in digital technology. For example, on the premise of not causing great discomfort to patients, a combination of digital scanning technology and traditional impression methods is used to obtain the information in the patient’s mouth.
(3) Actively explore and innovate the bio-materials used for 3D printing, seeking materials with good aging resistance, not easy to change color, low cytotoxicity, and excellent biological properties.
(4) Improve the application effect evaluation system to obtain the use and wearing situation of patients more accurately.
References:
[1] 王洋,王育新,张诗雷,俞青,卢晓林,杨旭东.3D打印赝复体即刻修复BrownⅡ类缺损的临床初步研究[J].中华整形外科杂志,2018,34(03):218-223.
[2] 周恬,顾晓宇.数字化和传统方法制备上颌骨缺损赝复体的效果评价[J].
[3] 王勇.口内数字印模技术[J].口腔医学,2015,35(09):705-709+743.
[4] 曹悦,陈俊锴,赵一姣,等.口内三维扫描技术临床应用精度的研究进展[J].中华口腔医学杂志,2020(03):201-202-203-204-205.
[5] Bidra AS, Taylor TD, Agar JR. Computer-aided technology for fabricating complete dentures: systematic review of historical background, current status, and future perspectives[J]. J Prosthet Dent, 2013, 109:361-366.
[6] 杜宝霞,王晓容,尹国相,等.3D打印预制赝复体即刻修复上颌骨前部缺损[J].口腔医学研究,2018,34(1):56-59
[7] Hu Y,Liu J,Wu W,et al.Immediate reconstruction of defects after a partial maxillectomy with a digitally planned,prefabricated,3-dimensionally printed,esthetic obturator prosthesis [J].J Prosthet Dent,2023:S0022-3913(23)00064-1.
[8] Zhao R,Dong Y,Liu N,et al.A digital workflow for fabricating an interim obturator after partial maxillary resection [J].J Prosthet Dent,2022:S0022-3913(22)00696-5.
[9] Elbashti ME,Hattori M,Patzelt SBM,et al.Feasibility and accuracy of digitizing edentulous maxillectomy defects:A comparative study [J].Int J Prosthodont,2017,30(2):147-149.
[10] Ye H,Ma Q,Hou Y,et al.Generation and evaluation of 3D digital casts of maxillary defects based on multisource data registration:A pilot clinical study [J].J Prosthet Dent,2017,118(6):790-795.
[11] 张晗之,朱陈元,谢雪梅,等.全数字化上颌赝复体制作与适合性初探[J].口腔材料器械杂志,2024,33(02):95-99.
[12] 刘苗,李风兰.数字化技术在上颌骨缺损赝复体修复中的应用[J].口腔医学研究,2024,40(05):385-388.DOI:10.13701/j.cnki.kqyxyj.2024.05.002.
[13] Koyama S,Sato N,Mito T,et al.Hermeticity of a hollow obturator model using CAD and rapid prototyping technologies [J].J Prosthet Dent,2020,124(1):123-127.
[14] 白石柱,张生睿,钟声,等.3D打印及其在口腔医学医学中的应用(一)——3D打印技术的工作原理[J].实用口腔医学杂志,2022,38(1):136-140.
[15] Karasan D,Legaz J,Boitelle P,et al.Accuracy of additively manufactured and milled interim 3-unit fixed dental prostheses [J].J Prosthodont,2022,31(S1):58-69.




Leave a Reply