Source: Modern Medicine and Health
Authors: Liu Xiaoyu, Ruan Xiaohui
Fixed orthodontics, as the main treatment method for orthodontic treatment, relies on the effective bonding of brackets to tooth surfaces. Whether brackets can be firmly bonded to tooth surfaces determines whether orthodontic forces can act on teeth and jawbones. Invisible orthodontics, as an emerging treatment method, has become increasingly accepted by the public due to its aesthetic, convenient, and comfortable features. The effectiveness of invisible orthodontics relies on the bonding performance of attachments to tooth surfaces, making attachment bonding a crucial foundation for invisible orthodontics. Therefore, tooth surface bonding is essential in orthodontic processes.
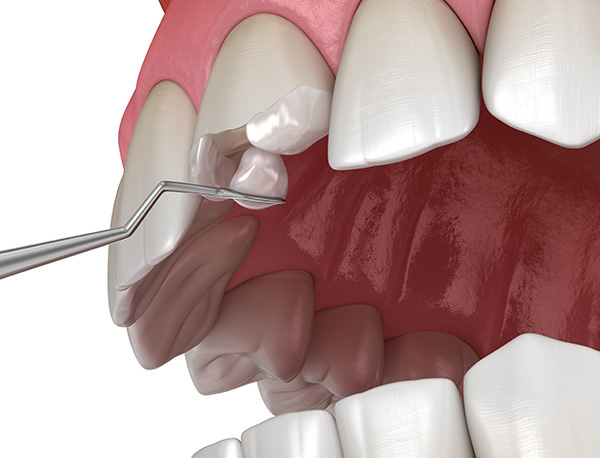
1. Principle of Tooth Surface Bonding
In 1966, acid etching was used for bracket bonding, where all adhesive systems are resin-based materials that adhere to the enamel on one side of the interface and bond to the material on the other side through a copolymerization process at the adhesive-composite interface. Tooth surface bonding adopts either total etch or self-etch adhesive systems. Total etch systems involve thorough acid etching of the tooth surface, creating a honeycomb-like micro-porous layer. Meanwhile, self-etch systems mix acid etchants and coupling agents without removing the smear layer but modifying it to form part of the resin tags that connect the resin to tooth tissues. Acid etching polarizes the enamel surface, dissolves enamel structures, and increases contact area and friction coefficient with the bonding agent through micro-mechanical interlocking. Over-etching can damage the enamel layer, reducing enamel strength.
Zhang Zeyu and others studied the effect of different acid etching times on bracket bonding strength in extracted tooth experiments, demonstrating no statistically significant difference in bracket bonding strength after 30s and 60s of acid etching of enamel. Clinically, choosing a 30s acid etch ensures adequate bracket bonding strength while minimizing enamel damage. Domestic scholars found increasing acid etchant concentration and time during enamel acid etching did not increase bonding strength. Instead, it caused more damage to young permanent teeth.
Both light-cured and chemically cured systems require enamel acid etching. Changes in specific operational times and procedures can impact bonding efficacy. Researchers conducted experiments on 60 extracted teeth using light-cured and chemically cured systems, prolonging acid etching time and soaking teeth in saliva after acid etching. The results indicated that extending acid etching time and delayed bracket curing weakened bracket bonding strength in light-cured systems, while soaking teeth in saliva after acid etching in chemically cured systems increased bonding strength.

2. Tooth Surface Treatment
The tooth surface, with a thin film of several micrometers thick, harbors proteins, bacteria, and lipids that hinder bracket bonding. Research on tooth surface cleaning agents conducted in vitro and in vivo confirmed that using BISCOVER LV liquid polish did not affect bracket bonding, implying no increase in bracket detachment rates. It also did not increase post-bracket removal damage but enhanced caries prevention.
2.1 Sandblasting of Tooth Surfaces
Sandblasting roughens tooth surfaces, enhancing resin adhesion. It involves high-pressure spraying of aluminum oxide, silicon dioxide, and other fine particles onto enamel surfaces, creating surface roughness that allows direct bracket bonding without acid etching. However, DARATSIANOS held different views, contending that sandblasting could not replace acid etching. Experimental results showed that sandblasting reduced shear bond strength by approximately 67% compared to acid etching and left less residual resin on teeth after detachment.
Researchers compared acid-etched and sandblasted tooth surfaces, proving that sandblasting increased bracket bonding strength but substantially damaged enamel. This finding corroborates with PATCAS, showing that sandblasting significantly alters enamel surface, making it rougher and removing more enamel compared to acid etching. The resin infiltration level and bonding strength remained the same with added sandblasting, but bonding strength increased.
2.2 Laser Etching
Laser etching, an alternative to acid etching, has been proposed for surface roughening. Previous studies revealed that phosphoric acid or Er, Cr:YSGG laser surface treatments improved the bond strength between traditional glass ionomer cement and composite resin. However, only laser etching significantly enhanced bonding strength in resin-modified glass ionomer cements.
SHAFIEI demonstrated that using 60mJ or 80mJ Er, Cr:YSGG laser treatment increased bonding strength without impact. Increasing laser energy, however, significantly reduced the strength enamel could withstand.
2.3 NaOCl Treatment of Tooth Surfaces
ARAS treated primary, young permanent, and mature permanent teeth with NaOCl, finding increased bonding strength in brackets after NaOCl treatment of young permanent teeth, possibly due to their loose and porous structure and abundant unmineralized proteins. The effects of NaOCl treatment did not differ in mature permanent teeth, and results on deciduous teeth were contentious.
3. Selection of Adhesive Systems
3.1 Chemically Cured Adhesive Systems
Early studies indicated that chemically cured adhesives provided greater bond strength than light-cured composite resins and resin-modified glass ionomer cements. However, the main drawback of chemically cured adhesives is their short setting time, which requires high technical precision during bracket positioning and is susceptible to air bubble entrapment, affecting bonding strength.
3.2 Light-Cured Adhesive Systems
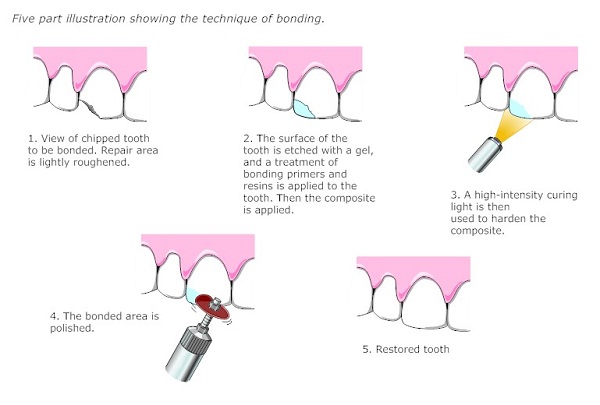
Light-cured adhesive systems primarily consist of resin composites that polymerize by absorbing energy from photo initiators, creating free radicals that undergo polymerization reactions. To avoid harmful effects of UV light on mucosa, visible light has been developed for curing. Attachments are typically made from light-cured resin used in tooth restoration, ensuring adequate strength and aesthetics. Evaluating attachment bonding strength is akin to assessing the bonding strength of adhesive systems on tooth surfaces.
Gu Yueguang and others compared the immediate and one-year damage and detachment rates of attachments made with flowable and compact resins in invisible orthodontics, affirming that flowable resin had greater attachment strength with shorter operation times. Yuan Ting and others similarly compared the initial attachment bonding effectiveness of flowable and compact resins, concluding that flowable resin outperformed compact resin. Observation with an intraoral scanner showed minimal defects in attachments bonded with flowable resin. However, foreign literature comparing the bonding strength of Z350 composite resin and Z350 flowable resin for attachment production indicated that the latter had higher operational ease, while both showed similar bonding strength.
Han Lei and colleagues compared Z350 nano-filled resin, Z350 nano-flowable resin, porcelain-filled resin, and porcelain-flowable resin for attachment stability and chairside operation time in invisible orthodontic treatments, suggesting the ease of operation and shorter chairside time with flowable resins, though long-term stability was better with nano-filled resins.
Xu Xiang conducted a clinical trial comparing the clinical outcomes of brackets bonded with total etch adhesive, self-etch adhesive, and resin-reinforced glass ionomer cements, finding no statistically significant difference in detachment rates among the three. Although resin-reinforced glass ionomer cements still exhibited a 10% detachment rate, their production time was shorter compared to other acid etch resin adhesives.
Chen Wener et al. conducted an in vitro study using Z350 universal resin, Z350 flowable resin, and SonicFill ultrasonic resin, concluding that SonicFill resin had higher shear strength than the other two, with flowable resin showing slightly lower strength. Additionally, flowable resin exhibited greater volume changes in attachments and occasional material overflow onto tooth surfaces compared to the easy operability, short operation time, and strong bonding strength seen with SonicFill resin.
3.3 Comparative Studies of Light-Cured and Chemically Cured Adhesive Systems
Li Hanling and others conducted comparative experiments on 32 extracted premolar teeth, testing shear forces after bonding brackets with traditional chemically cured and light-cured resin adhesives, finding that light-cured resin had stronger bonding strength. However, there was no statistically significant difference in the residual resin area on tooth surfaces after bracket removal between the two groups. Mo Yinhe and others compared 3M chemical adhesive, 3M light-cured resin adhesive, and Hangzhou West Lake adhesive for bracket bonding, also concluding that the bonding strength of the 3M light-cured resin adhesive was higher than the other two.
Foreign researchers compared high-viscosity glass ionomer cements, resin-modified glass ionomer cements, flowable composite materials, and conventional flowable composite materials for bonding strength to tooth surfaces. While each group exhibited good bonding strength at the bonding interface, high-viscosity glass ionomer cements modified with MPC had higher bonding strength than other materials when self-etched.
Liu Gang and colleagues compared the bonding strength and residual amount of light-cured resin adhesive and light-cured resin-reinforced glass ionomer cement in an in vitro experiment, finding that the light-cured resin adhesive had greater bonding strength and more residual bonding material after bracket removal than the light-cured resin-reinforced glass ionomer cement, indirectly indicating that the light-cured resin adhesive better protected enamel during bracket removal.
3.4 Modified Adhesive Systems
Park Xiu Lu et al. added different concentrations of 2-methacryloyloxyethyl phosphorylcholine (MPC) to adhesive systems to investigate the effect of modified self-etch adhesives with MPC on bonding strength, finding no impact on bracket bonding strength with 3.0% to 7.5% MPC concentration. While some researchers suggest that adding MPC to adhesives enhances enamel protein adhesion resistance and bacterial adhesion prevention, it may not provide a definitive advantage for bracket bonding to enamel.
White spot lesions (WSLs) are common complications in orthodontic treatment, often occurring on maxillary incisors and canines. WSLs present as whitish chalky spots on enamel surfaces due to demineralization, increasing the risk of tooth decay. To reduce tooth decay after bracket bonding, many researchers have studied the use of antimicrobial agents in adhesive systems. For instance, Qu Lu Lu et al. incorporated different concentrations of the quaternary ammonium monomer methacryloyloxydodecylpyridinium bromide (DMAHDM) into flowable resin, demonstrating that 7.5% DMAHDM in adhesive materials had the lowest bacterial adhesion while reducing shear strength, implying decreased bonding strength. Although meeting orthodontic bonding requirements, it may not ensure long-term stability in bracket bonding.
Li Zhenxia and colleagues conducted an in vitro study on the effect of nano titanium dioxide on the antibacterial properties and tensile bonding strength of light-cured orthodontic bracket adhesive (Grengloo). Light-cured resins used in clinical orthodontic treatments were mixed with various mass fractions of nano titanium dioxide, showing that the adhesive material exerted some antibacterial properties without affecting bonding strength.
4. Curing Light Intensity
Some researchers propose that different LED light intensities in light-cured resin adhesive systems can affect bonding strength, especially for older LEDs with diminished intensity that may not achieve the necessary resin bonding strength level when exposed for a similar duration, while the brand of LEDs showed no statistically significant difference in bonding strength regardless of light intensity.
PHANEUF et al. suggested using polystyrene strips to delay light-cured resin curing to investigate bracket bonding strength under normal oral conditions and anaerobic intervention conditions. The study concluded that anaerobic conditions did not significantly affect bonding strength but increasing the adhesive material thickness did impact bonding strength.
5. Anatomical Position
Clinical operations in the oral cavity may not always achieve 100% operational standards, impacting bracket and attachment bonding efficiency. Due to anatomical positioning, brackets and attachments in the posterior teeth region pose greater operational challenges, prolonging operation time and potentially altering the physicochemical properties of bonding agents, affecting bracket bonding strength. Additionally, lower detachment rates in lower teeth may be attributed to poor moisture isolation, leading to saliva contamination during bonding and reduced bonding strength. Furthermore, posterior tooth attachments were more likely to detach compared to anterior teeth due to poor moisture isolation and operational difficulties.
6. Patient Factors
Brackets are located in the oral environment, where inadequate oral hygiene maintenance by patients can lead to bacterial plaque accumulation around brackets on uneven tooth surfaces, causing localized demineralization. This not only increases the risk of tooth decay but also reduces shear forces the area can withstand, affecting bracket and attachment bond strength. Children exhibit higher bracket detachment rates than adults, as some children undergoing orthodontic treatment may have stronger parental demands, lack awareness of the importance of oral hygiene, exhibit poor compliance, and neglect dietary and daily habits, resulting in higher detachment rates.
As orthodontic treatment progresses, patients’ discomfort, desire for aesthetics and health, and improved compliance gradually result in better cooperation with doctors, increased focus on oral hygiene, and subsequently reduced bracket detachment rates. In invisible orthodontics, the frequency of patient-initiated removal of appliances also impacts attachment detachment rates, with detachment rates increasing when the appliance is removed five or more times a day. Choosing to wear orthodontic devices while eating can inhibit attachment detachment.
7. Conclusion
In conclusion, dental bonding technology continues to evolve, with bonding strength affected by various factors. To maximize the mechanical interlocking effect of enamel surfaces, cleaning and tooth surface treatment are essential. Tooth surface cleaning involves removing lipids, proteins, bacteria, and plaque, while tooth surface treatment enhances roughness, increases the bonding area with adhesive, and enhances bonding strength.
Methods to increase tooth surface roughness include sandblasting, laser etching, chemical treatment, all of which achieve surface roughening effects. However, tooth surface treatment cannot replace enamel acid etching. Acid-etched tooth surfaces create a honeycomb-like micro-porous layer where resin tags and enamel form mechanical interlocks. The selection of adhesives is also crucial in determining bonding efficacy.
With advancing technology, various adhesive systems have been introduced. Light-cured adhesives are convenient, quick, and offer sufficient bonding performance, hence widely used in clinical practice. Incorporating caries prevention and antibacterial agents into adhesives can prevent cavities without compromising bonding efficacy. The curing initiating condition of light-cured adhesive is light exposure, with light intensity being a crucial factor affecting bonding strength. Older light-curing lamps that do not meet curing requirements can impact bonding efficacy.
Additionally, anatomical location and patient factors influence bracket and attachment bonding on tooth surfaces. Anatomical positioning complicates bracket and attachment bonding in posterior tooth regions, leading to reduced moisture isolation, prolonged operation time, and inferior bonding efficacy. Patient oral hygiene maintenance guarantees maximum bonding strength of brackets and attachments post-bonding. In invisible orthodontic treatments, patients are advised to minimize appliance removal frequency to reduce attachment detachment rates and improve tooth movement efficiency.




Leave a Reply