Authors:
Hari Petsos, M. Sc. (Contact Person) (Germany)
Periodontology Clinic, Oral and Maxillofacial Treatment Center, Frankfurt University
Oral and Maxillofacial Surgery Clinic
Dr. Jörg Korte (Germany)
Oral and Maxillofacial Surgery Clinic
Frank Fleckenstein, M. Sc. (Germany)
Dental Clinic
Professor Peter Eickholz
Periodontology Clinic, Oral and Maxillofacial Treatment Center, Frankfurt University
A 58-year-old female patient was found to have extensive severe chronic periodontitis during her initial examination. To preserve most of her teeth, multidisciplinary and multi-professional combined treatment was needed. The patient wished to restore her missing teeth with fixed prostheses and to replace her old crowns for aesthetic purposes. This treatment goal was achieved through mutual trust and good cooperation between general practitioners and specialists. This case is published in two parts. The first part mainly discussed the clinical examination results, diagnosis, treatment plan, and pre-implantation treatments (see Issue 5 of the Comprehensive Edition). This second part focuses on implant placement and restoration.
This article is published in two parts, with this being the second part, and the first part was published on November 15, 2024.
Implant Treatment (Specialist)
Due to progressive resorption of the alveolar bone in quadrants III and IV, a navigated approach was chosen for implant placement. This reverse planning method not only achieves an ideal restoration position but also determines large autogenous bone donor areas. This approach allows for significant bone augmentation while avoiding damage to the inferior alveolar nerve. Therefore, the implant planning software from SICAT (Germany) was used. After placing an imaging guide on the patient, a CBCT scan was taken for implant planning.
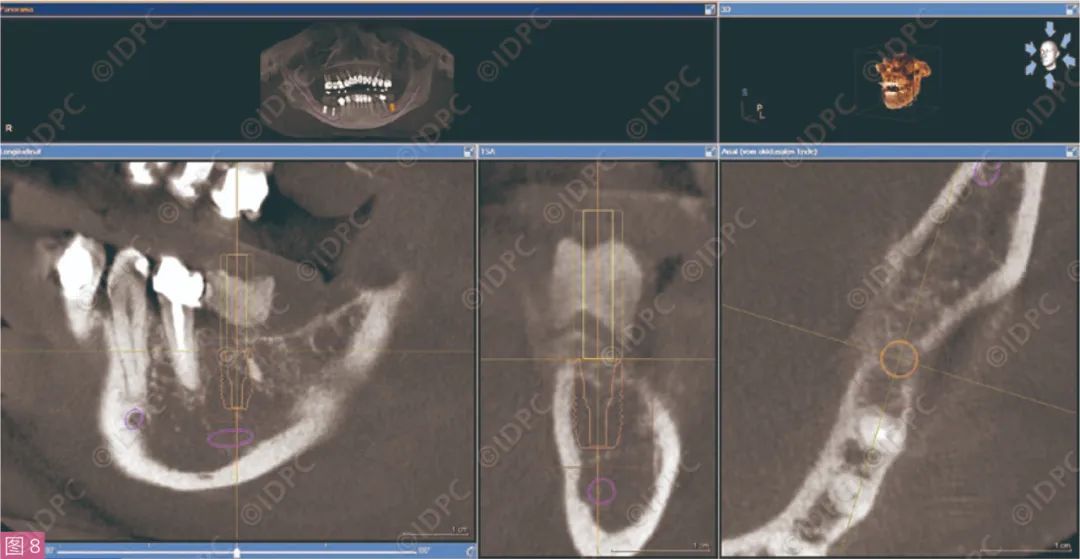
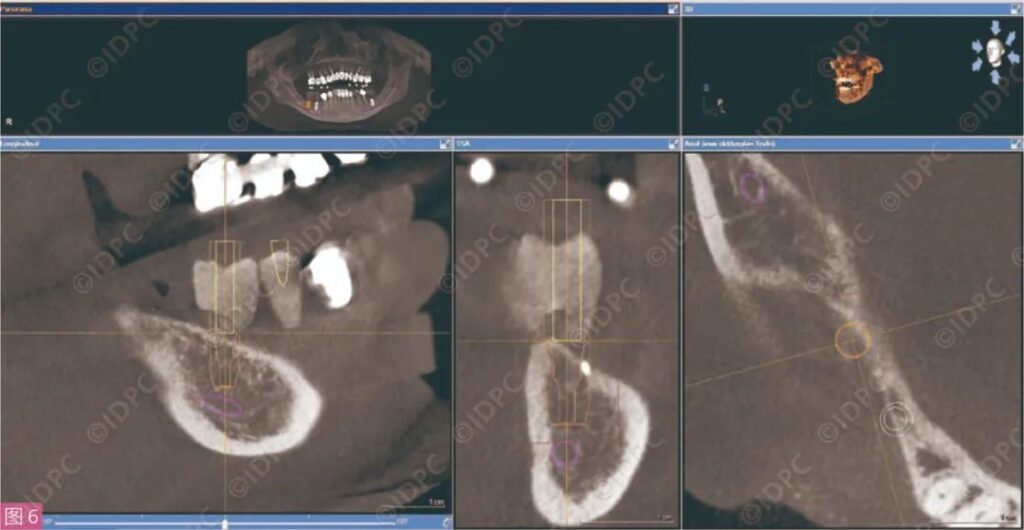
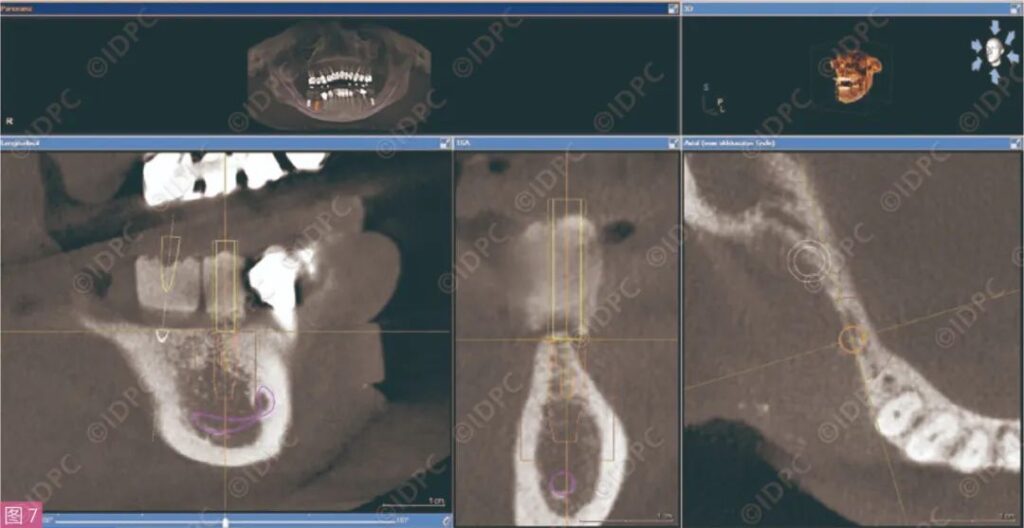
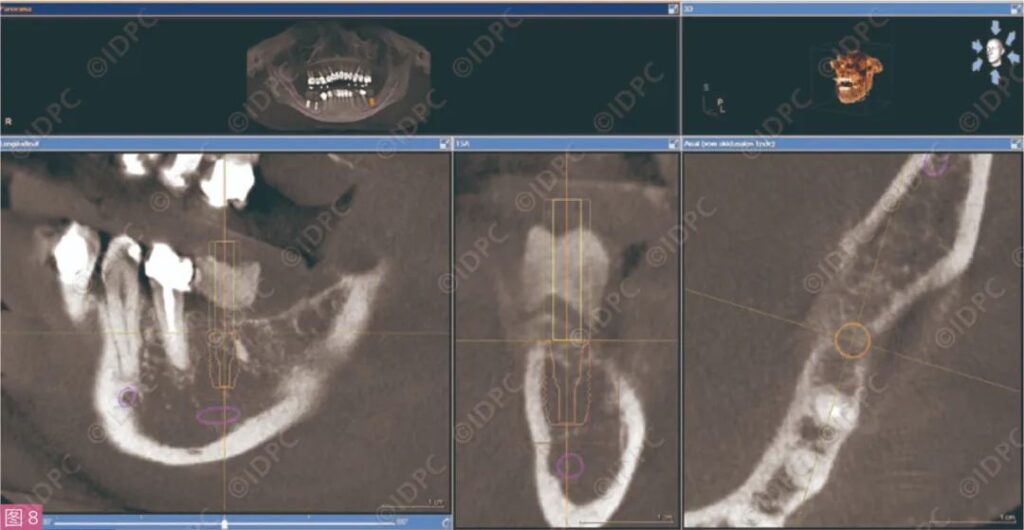
First, the position and course of the inferior alveolar nerve canals on both sides of the mandible were marked on the CBCT images (marked in purple). Then, based on the denture conditions provided by the imaging guide and the existing bone conditions, the implant placement positions were determined (in orange) (Figures 6 to 8). To ensure the implant (Astra Tech Osseospeed TX S, Dentsply, Germany) is represented by an orange rectangle in the CBCT images, a safety distance of 1.5mm was maintained. The position of the implant at site 46 needed to ensure that foreign objects within the bone could be removed without irritation during bed preparation (refer to Figure 6). Given the inclination of the mandibular bone resorption in the fourth quadrant and the course of the inferior alveolar nerve, it was decided that the buccal part of the implants at sites 45 (refer to Figure 7) and 46 (refer to Figure 6) would slightly be above the ridge with lateral bone augmentation. For the implant placed at site 36, there was sufficient safety distance from the inferior alveolar nerve, allowing for planning without bone augmentation (refer to Figure 8). Finally, this data was sent to the software company to produce a personalized implant guide (OPTIGUIDE, SICAT Germany) and form related implant procedure guidance.
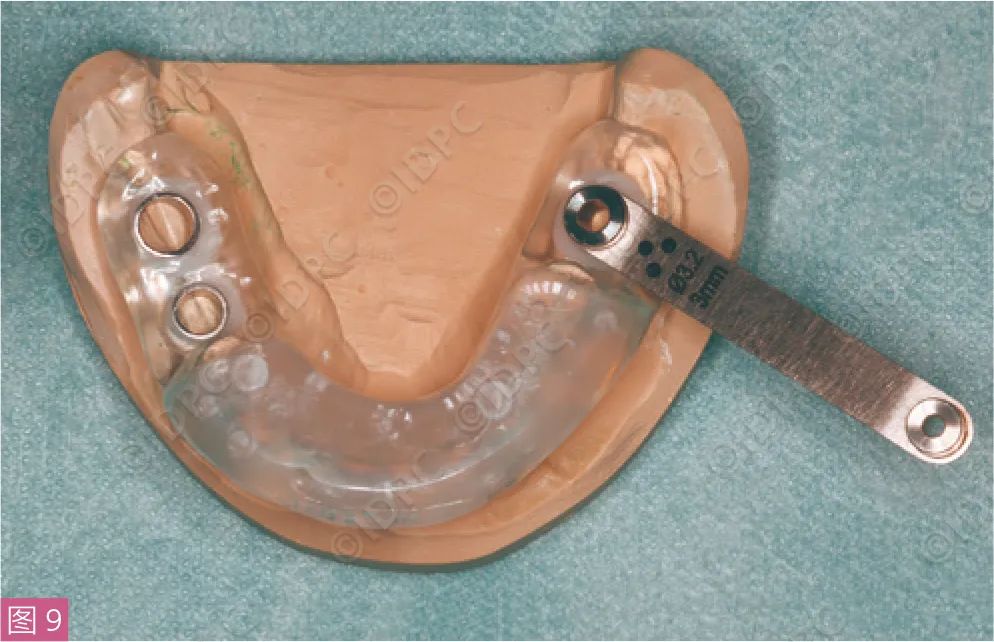
On January 16, 2015, under the guidance of the implant guide, implants were placed at sites 36, 45, and 46, with simultaneous lateral bone augmentation in regions 45 and 46 (Puros Allograft, Zimmer Biomet Dental USA) covered with a biological membrane (Copios Pericardium Membrane, Zimmer Biomet Dental, USA). Under local anesthesia, a mid-crestal incision was made at the alveolar crest without releasing incisions. A full-thickness flap was elevated with a periosteal elevator, and a tooth-supported implant guide was placed (Figure 9). The bed was prepared with depth markers and various sleeves (Facilitate, Dentsply Sirona Implants, Germany) according to the guide. Finally, the implant was mechanically inserted through the implant guide (Astra Tech Osseospeed TX S 5.0 x 9mm) with a cover screw used to close it. Interrupted sutures (SABApol 5-0, SABANA, Germany) closed the incision.
A similar procedure was prepared for a mucoperiosteal flap at sites 45 and 46, but with vertical releasing incisions mesially and distally, along with a periosteal incision to ensure tension-free closure after augmentation. The implant at site 45 (Astra Tech Osseospeed TX S 4.0 x 11mm) and the implant at site 46 (Astra Tech Osseospeed TX S 5.0 x 9mm) were mechanically inserted and closed with cover screws similarly. After implantation, several holes were drilled in the cortical bone, and a loose allograft replacement material was placed over the exposed buccal surface of the implants, then covered with a biological membrane.
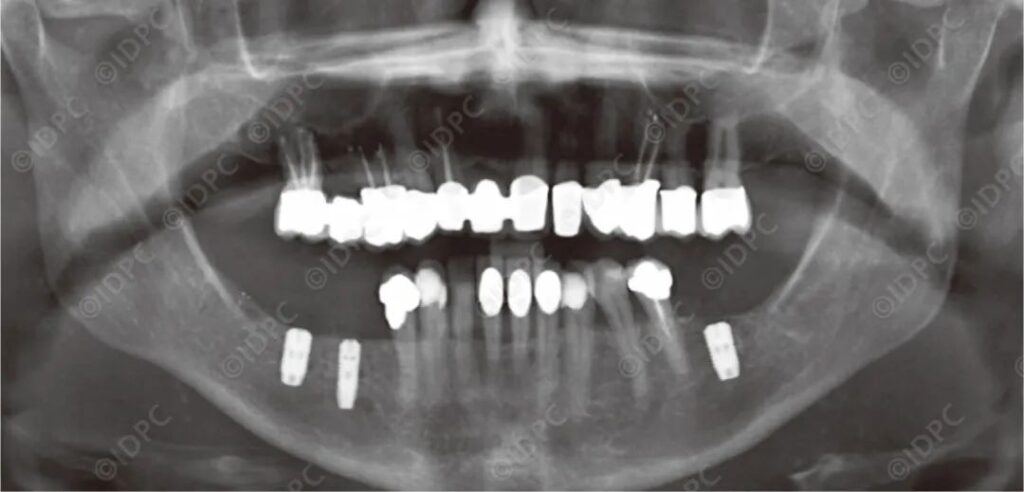
The mucoperiosteal flap was repositioned, and horizontal mattress sutures were used to align the incision edges, with interrupted sutures to achieve tension-free closure (Figure 10). A panoramic radiograph was taken afterward (Figure 11). The patient was instructed to rinse twice daily with 0.12% CHX solution for about 2 minutes and to apply 1% CHX gel to the wound several times a day after oral cleaning for two weeks. The patient was advised to allow the fourth quadrant incision to heal with minimal stress and therefore no temporary dentures were used. Additionally, the patient took antibiotics (300mg clindamycin) three times daily for five days and analgesics (Ibuprofen 600mg) as needed. Sutures were removed 14 days after the implants were placed.

Implant Exposure (Specialist)
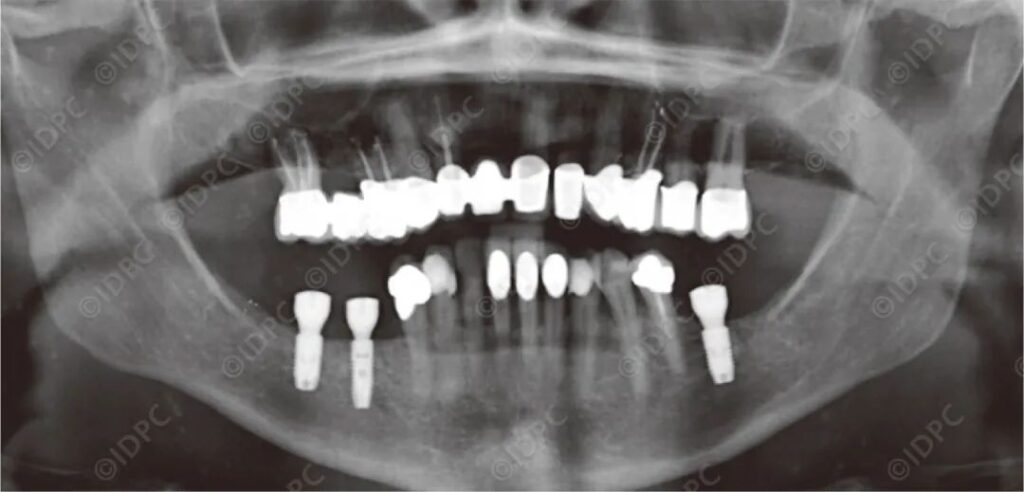
On June 11, 2015, after a four-month healing period, the implants were exposed. Under local anesthesia, a slightly lingually oriented crestal incision was made in the fixed mucosa above the implants, without releasing incisions, and a half-thickness flap was elevated with a periosteal elevator. The cover screws were removed, and appropriate gingiva formers were tightened by hand. A postoperative panoramic X-ray was taken (Figure 12). Based on the implant condition and postoperative performance, antibiotics were considered unnecessary.
Mandibular Prosthesis Restoration (General Practitioner)
By September 15, 2015, the current long-term temporary dentures were replaced with formal restorations. Customized zirconia abutments and titanium bases (Ceramill Zirkonia on Ceramill Ti-Form, Amann Girrbach, Austria) were cemented, and full-ceramic single crowns were temporarily cemented. The screw channels were sealed with cotton pellets and temporary, low-hardness, light-curing composite filling material (TempBond, Kerr). Teeth 35-44 were also restored with full-ceramic single crowns, temporarily cemented with TempBond. During a follow-up examination on September 11, 2015, gingival healing was good, with no inflammatory irritation, and the aesthetics were very satisfactory to the patient. The full-ceramic crowns on teeth 35-44 were permanently cemented with PANAVIA™ V5 (Kuraray).
Evaluation and Prognosis
The preoperative diagnosis of chronic periodontitis was related not only to the patient’s age (at the time of diagnosis, this female patient was 58 years old) but also to local factors contributing to the extent of destruction. For this particular case, during the initial examination on October 15, 2013, most of the patient’s teeth had been restored with dentures, and probing parameters and periodontal attachment loss had increased. The initial PCR value of 40% confirmed these, with positive sites not located in the restoration margin area. Additionally, visible calculus on X-rays was found on vulnerable parts of the mandibular anterior teeth, related to local irritant factors. Tooth-associated local factors, such as root bifurcation lesions, can similarly exacerbate periodontal destruction. No conclusions could be drawn about the progression of periodontal lesions, as only X-rays from 2013 were available.
This patient had extensive severe chronic periodontitis, with more than 30% root surface attachment loss ≥5mm at the initial examination.
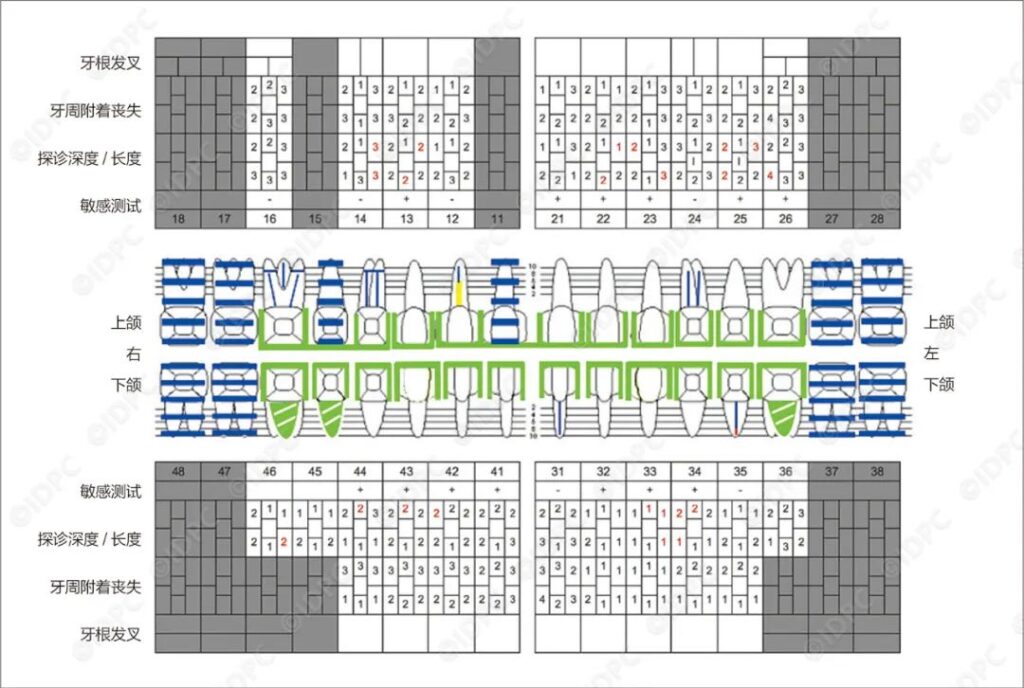
Upon clinical reevaluation of the intraoral situation, only teeth 14, 13, 21-23, 31, and 41 showed probing depths of 4mm with bleeding on probing (BOP) or probing depths of 5mm (see Figure 5). Periodontal pockets with probing depths ≥5mm are associated with an increased risk of progressive periodontitis. To further eliminate periodontal pockets, flap surgery was not chosen, as a seven-year observation showed no advantage compared to conventional scaling and root planing (SRP) for 5mm pockets. Due to the lack of evidence-based medicine, root bifurcation regeneration treatment was not performed on tooth 16. Root bifurcation lesions of degree I on teeth 16, 14, and 26 did not require further treatment. Over 11 months of observation, they remained stable and closed.
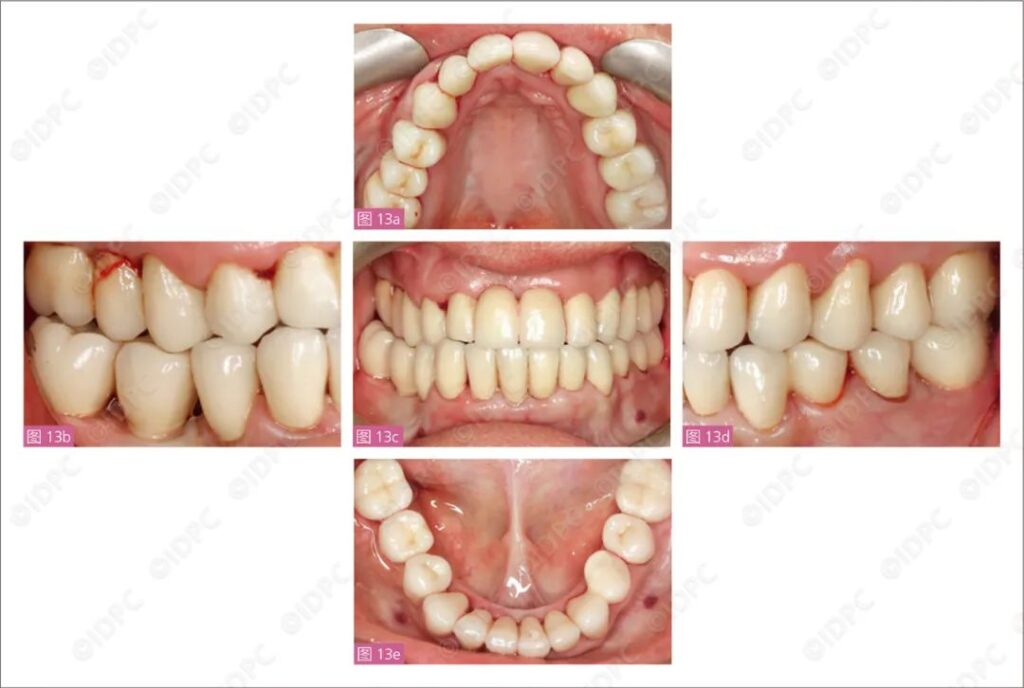
Improved examination results at reevaluation were crucial for remaking the maxillary restorations. To maintain periodontal stability, restorations should be designed to facilitate oral hygiene maintenance (Figure 13).
During the second periodontal maintenance treatment on November 3, 2014, no periodontal pockets with probing depths ≥5mm were present. Local probing depths of 4mm with bleeding on probing remained on teeth 13, 21, 22, 31, and 41, which were controlled and re-debrided through periodontal maintenance treatment.
This female patient did not smoke, but had a positive history of periodontitis. She was pre-informed about the risks of implant treatment.
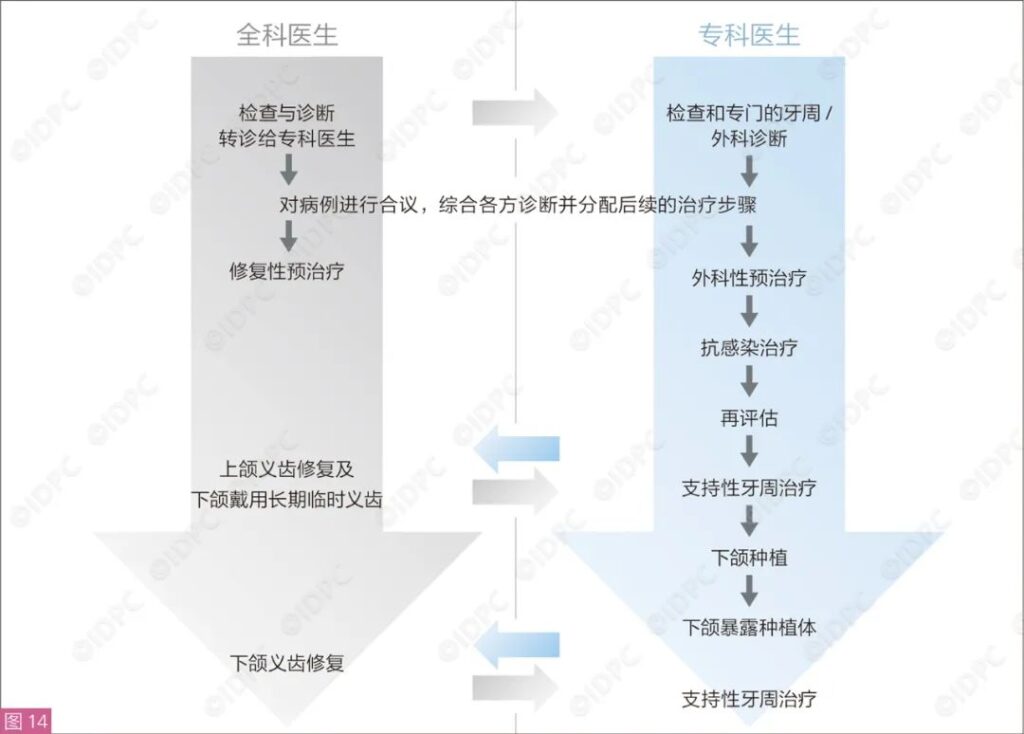
After confirming the stability of the periodontal condition, implant preparation began. Guided implant placement was chosen due to proximity to the inferior alveolar nerve (canal). The formal mandibular prosthesis restoration considered both treatment needs and the patient’s desires. Tasks between specialists and general practitioners were clearly defined (Figure 14), and despite the significant time and cost investments, stable and satisfactory results have been achieved so far. Such ideal and comfortable mandibular prostheses could not have been provided without the cooperation among the experts. Additionally, if a removable telescopic crown prosthesis had been chosen for the mandible instead of fixed dentures, tooth 35 would also need to serve as an abutment. However, this tooth had inadequate endodontic treatment, and as the most distal abutment, there was a risk of fracture under the long-term load of a free-end denture.
Compared to the initial examination, periodontal conditions have objectively improved (Figure 15). The patient’s desire to retain as many teeth as possible and obtain aesthetically pleasing new maxillary prostheses from her perspective has also been fulfilled.
At the beginning of treatment, the long-term retention of teeth 16, 32, 31, and 41 was considered uncertain: tooth 16 had a degree II distopalatal root bifurcation lesion with inadequate root filling and periapical bone resorption. Other problematic teeth had bone loss >50%, associated with increased risk of tooth loss. However, now inflammation has disappeared, and probing depths and periodontal attachment loss are less than 4mm. Ultimately, it cannot be determined that the tooth’s distopalatal root bifurcation lesion is degree II. Under periodontal maintenance treatment (UPT), periodontal conditions are well-controlled. Teeth 14 and 16 improved after root canal retreatment. Moreover, root canal treatment for teeth 24 and 31 was crucial for the final restoration, as it can extend the 5-year survival rate of fixed dentures to over 89%. Further periodontal maintenance treatments under specialist supervision, although increasing average costs, are associated with reduced tooth loss/peri-implantitis in the literature. At no point did the patient experience functional issues. From the patient’s perspective, previously unsatisfactory aesthetics were improved with the new prosthesis restorations, and she is absolutely satisfied with the restoration results.
— END —




Leave a Reply