
Authored by Todd R. Schoenbaum
Significance of Provisional Restorations
The theoretical basis for using immediate provisional restorations is that they can support and maintain the structure of the soft tissue around the implant. Maintaining the ideal soft tissue aesthetic form is easier than reconstructing collapsed soft tissue. Most patients prefer fixed provisional restorations, although special care must be taken to prevent overloading the implant or fracturing the provisional restoration. Before taking the final restoration impression, the provisional restoration can serve as a communication bridge between the doctor and patient regarding the appearance and function of the final restoration. If the provisional restoration does not meet aesthetic, functional, phonetic, or hygienic needs, it can be easily modified during the provisional stage. The provisional restoration can serve as a reference to anticipate the final restoration’s effect, allowing medical staff to make precise adjustments. This method significantly enhances the predictability of the final restoration. It is strongly recommended to use provisional restorations in all aesthetic zone implant treatments or other complex cases.

Fabrication of Provisional Restorations
Selection of Materials for Provisional Abutments
I recommend using titanium provisional abutments among the many provisional materials available. Some clinicians may hesitate when choosing materials because titanium abutments are slightly more expensive and harder to cut than polyether ether ketone (PEEK) or other materials. The fundamental reason for choosing titanium provisional abutments is their high mechanical strength. Titanium offers the best biocompatibility among current materials, which is crucial in the initial stages of soft tissue healing and osseointegration. It is unbreakable under normal use. We do not want the provisional abutment to fracture within three weeks of osseointegration. Titanium forms the optimal seal at the implant-abutment junction (IAJ), essential for maintaining bone stability around the implant. Materials with slightly less rigidity, such as PEEK, may allow micro-movement at the IAJ due to material flexion, potentially leading to bone loss around the implant. The gray color of titanium abutments can be masked with opacifying composite resin (Fig. 2). Titanium abutments can be trimmed using high-speed tungsten carbide burs, although this generates heat and sparks. Avoid intraoral trimming of titanium abutments and trim them in an environment with free oxygen flow. If the titanium abutment overheats during trimming, it can be submerged in water for cooling. A hemostat can be used for holding during trimming or connected to an abutment analog.

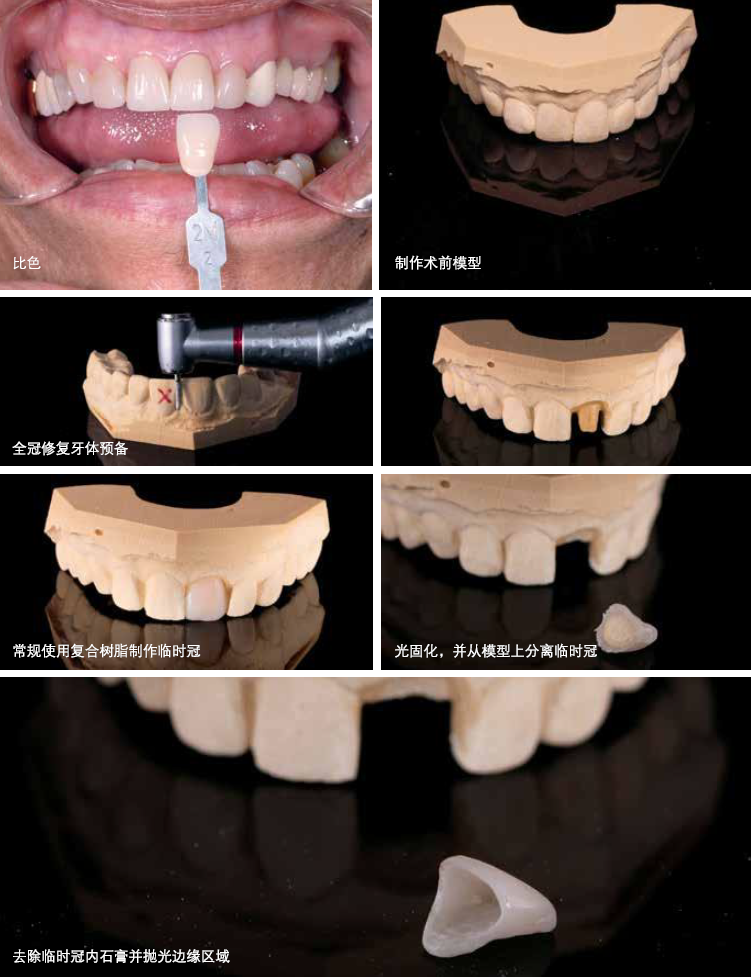
Selection of Materials for Provisional Crowns
The crown portion of the provisional restoration is preferably made by a technician. Provide the technician with an impression, model, or digital scan and the chosen color information. Instruct the technician not to remove the screw channel, as individual provisional crowns are typically made from composite resin, while polymethyl methacrylate (PMMA) is often used for multiple implant provisional restorations. The clinical restorative dentist will grind out the screw channel after the implant surgery. Compared to PMMA, composite resin promotes easier connection of the provisional crown to the provisional abutment at the implant site. Light-cured composite resin is easier and safer to work with than room-temperature cured PMMA materials. Regardless of the material used, a reliable bond between the provisional crown and the provisional abutment is required. Composite resin offers convenience, durability, lower porosity, and more stable color. Additionally, composite resin provisional crowns are easy to modify, shape, and repair. Light-cured composite resin provisional crowns are also convenient for adjustments in length, emergence profile, shape, and color; whereas PMMA is time-consuming and labor-intensive for such modifications (Figs. 3-4).

Key Points for Fabricating Multi-Implant Provisional Fixed Dentures
Immediate restoration can only be performed when the implant surgeon confirms sufficient initial stability of the implants. Clinicians with different educational backgrounds or training experiences may have different criteria for judging initial stability. Common methods include resonance frequency analysis (RFA), implant stability quotient (ISQ), insertion torque, and the clinician’s sense of touch. If the surgeon believes the implant’s stability is insufficient for implant-supported immediate provisional restoration, an alternative method for provisional restoration should be used. Long span or full arch provisional fixed restorations are essential for the restoration process of multiple implants. They provide comfort to the patient during osseointegration without the need for removable restorations. The design of provisional restorations can vary, requiring consideration of numerous factors, including the bone volume and location in the edentulous area, the smile line position, patient expectations, and the number and type of implants. The design scheme introduced here is suitable for most patients, with different materials available for various implant cases. Slight modifications may be necessary based on the patient’s specific situation. The multi-implant provisional fixed restoration described here shares some similarities with the previously described individual provisional fixed restoration, but there are also differences. Multi-implant provisional fixed restorations require a non-anti-rotation design. This means the abutment should not fully engage the anti-rotational connection within the implant. This allows for some degree of angulation between different implants, minimizing the likelihood of the abutment becoming locked due to rigid connection. When linking two or more restorations using a fixed dental prosthesis (FDP), anti-rotation features are unnecessary. Non-anti-rotation abutments minimize the potential for non-passive seating, which could lead to provisional restoration fracture, osseointegration issues, or even implant failure. Another difference between multi-implant and single provisional restorations is whether PMMA is used. As mentioned earlier, composite resin is superior to PMMA in nearly all relevant indicators (e.g., ease of use, control, color stability, porosity), yet contemporary multi-unit provisional restorations are made by digitally designing and milling suitable resin blocks. While multi-implant provisional fixed restorations (FDP) can be made by milling resin blocks, they are not yet widely used clinically. Clinically, PMMA is more commonly used, and the following sections describe the PMMA process. Since the provisional crowns are made from PMMA, similar materials are needed to connect the provisional crowns and abutments to avoid bonding failure. Therefore, powder/liquid mixed self-curing PMMA is used in the implant surgical area inside the mouth. Care should be taken to avoid contaminating the implant or graft materials. Small pieces of a rubber dam can help prevent material from entering the surgical area. The position of the provisional restoration is crucial for implant success when restoring multiple missing teeth with implants and performing provisional fixed restorations. There are several methods to determine the ideal occlusal vertical dimension (OVD). There are also various methods to determine the ideal position of teeth based on aesthetics and phonetic standards. Regardless of the method used, precise and complete transmission of this information to the technician is essential. Preoperatively, at least a facebow record and a complete set of facial diagnostic photographs are necessary. Simultaneously, patient expectations should be considered. Proper centric and lateral relationships should be personalized according to the patient’s actual situation. When making multi-implant fixed bridge (FDP) provisional restorations, the clinician can use “wings” (placed on remaining natural teeth), palatal straps (supported by immobile attached tissue on the palate, used for referencing restoration position), or locator clips to assist in transferring the position of the restoration. Note that if your team uses guided or navigational methods for implant surgery, the steps described here will need to be appropriately adjusted according to the specifics of the implant system you are using. Despite extensive efforts in fabricating multi-unit immediate FDP provisional restorations, it is still recommended to fabricate a second round of provisional restorations after osseointegration (two rounds of provisional crown fabrication). This allows for improvements to the restoration by clinicians and technicians before the final restoration. Notably, you may find soft tissue changes, tissue surfaces may need re-lining, papillae may need contouring, or red aesthetics may require repair. After osseointegration, discuss four key factors with the patient: (1) aesthetics; (2) phonetics; (3) function; (4) hygiene. If one or more of these indicators fall below patient desires and expectations, appropriate adjustments can be made during the second round of provisional restoration modifications, or other surgical interventions can resolve the issues. Once all parties are satisfied, the provisional restoration stage can conclude, and the final restoration can be crafted based on the satisfied, reliable provisional restoration used for several months (Fig. 5).





Leave a Reply