Abutments serve as the link between the implant and the restoration, and selecting the appropriate abutment is crucial for achieving optimal functionality, aesthetics, and long-term success in implant restorations. Compared to cast abutments, traditional standard or prefabricated abutments are more cost-effective and readily available, but they can lead to residual cement issues, resulting in biological complications and the inability to reuse the restoration, necessitating remanufacturing.
Regarding abutment materials, whether metal-ceramic (titanium/gold alloy) or all-ceramic (zirconia), the overall clinical outcomes are promising. Generally, zirconia abutments are relatively superior in aesthetics but come with some mechanical issues. In recent years, with the development of CAD-CAM technology, the selection of implant abutments has undergone significant changes. Customized CAD-CAM all-ceramic and titanium abutments have become very popular as they can be integrated into digital workflows, reducing time and manufacturing costs.
A systematic review published on June 12, 2024, in the journal “Clinical Oral Implants Research” (Clin Oral Implants Res) clearly outlines the selection of CAD-CAM abutments and restoration materials for implant-supported fixed restorations in patients with missing teeth. This article will summarize the section on abutment selection from the review for the reference of dental practitioners.

Implant Single Crown Abutment Selection
1.Titanium Base Abutment
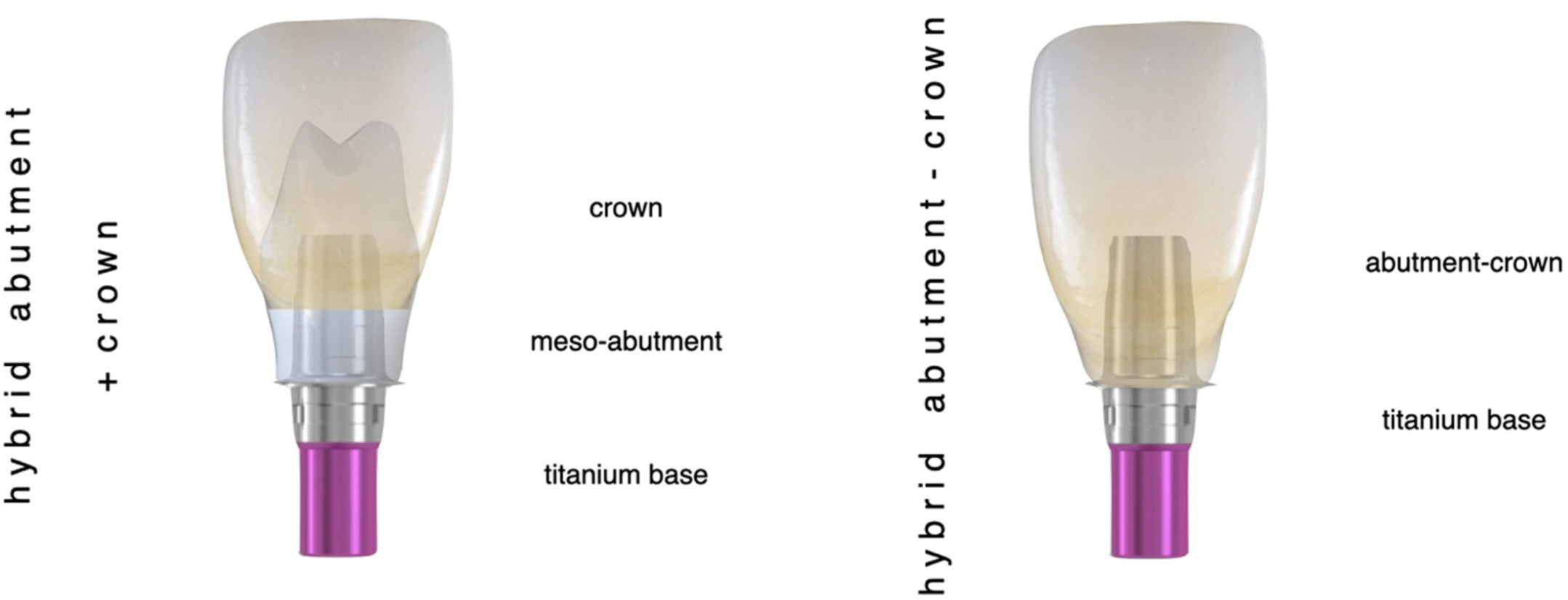
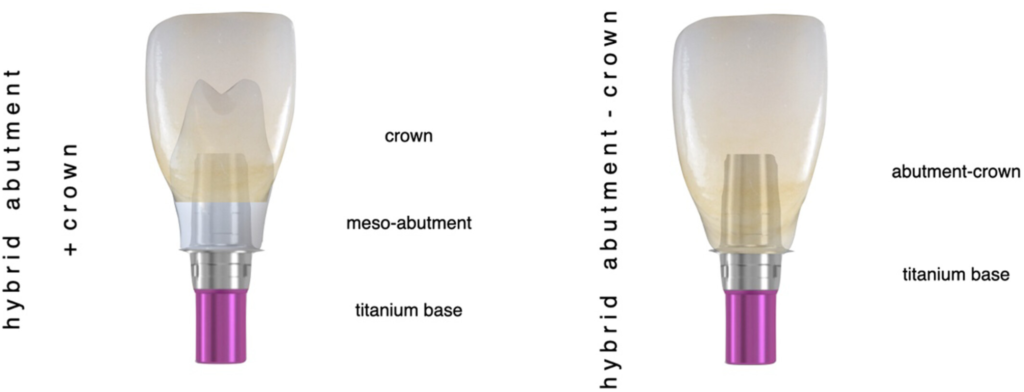
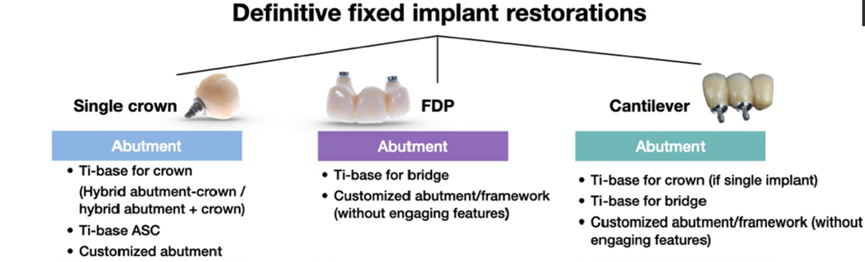
Titanium Base abutments are prefabricated standard abutments with anti-rotational features and relatively parallel walls, supporting customized all-ceramic abutments (composite abutments) or full crowns. In the first scenario, the customized all-ceramic abutment is cemented to the titanium Base outside the mouth, and then the entire unit is fixed with screws onto the implant and crown, forming an integrated screw-retained restoration. In the second scenario, the titanium Base is cemented to the full crown outside the mouth, and the entire unit is then fixed with screws onto the implant (Figures 1-3).
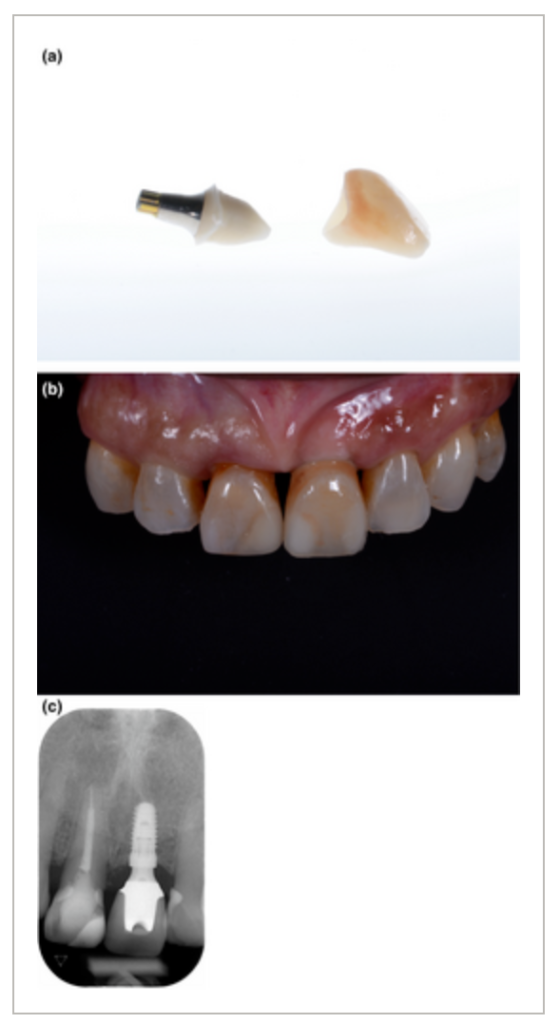
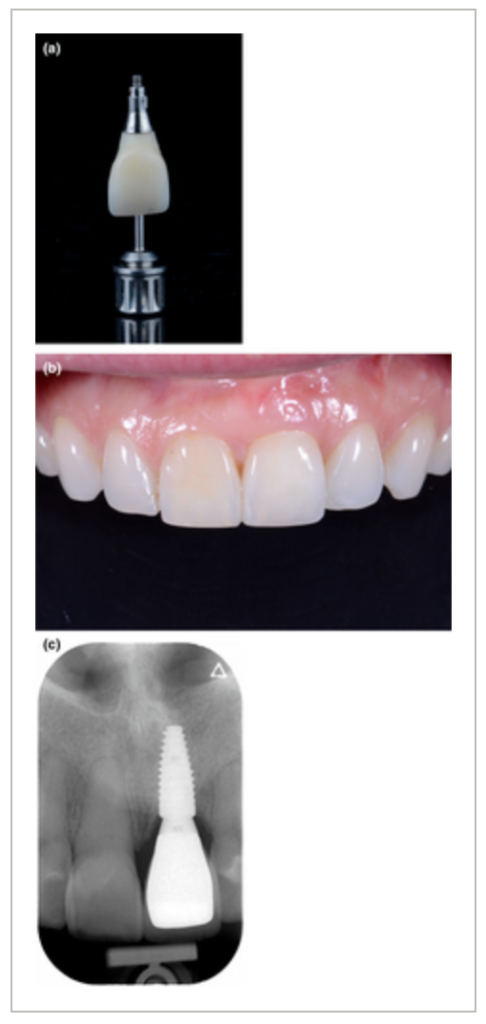
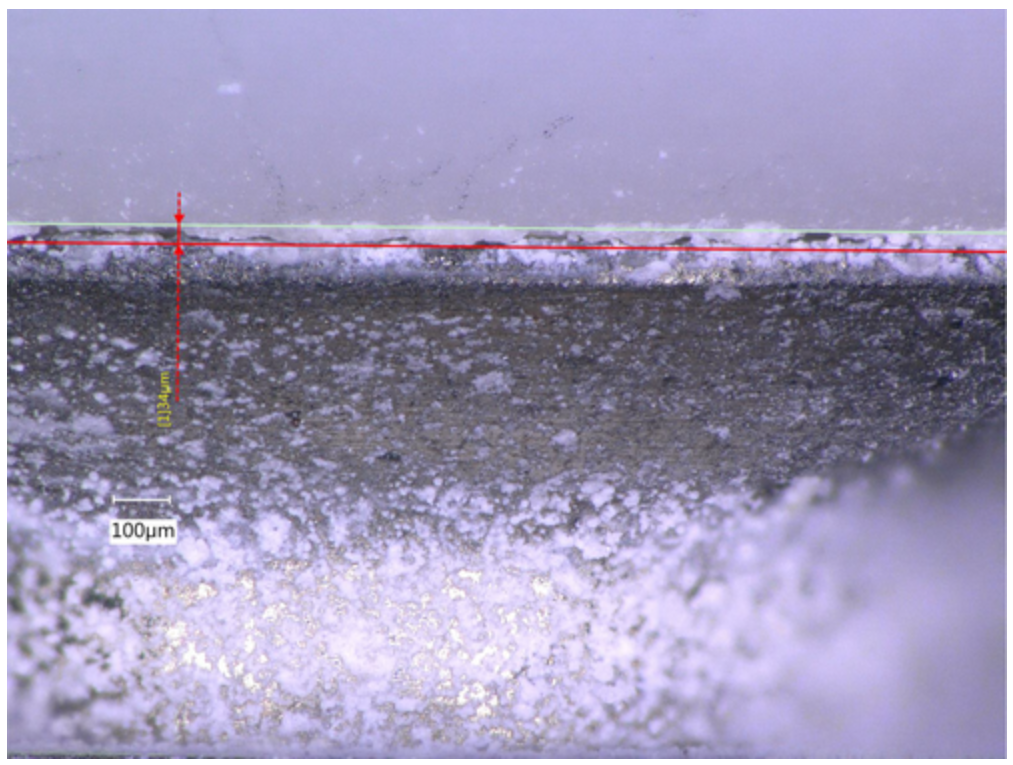
Compared to zirconia abutments, titanium Base offers both the mechanical stability of metal connections and aesthetic effects. Additionally, the titanium Base can be stably bonded with upper ceramics to withstand masticatory forces in the oral cavity. However, we often worry about the weak bonding interface between the titanium Base and the crown, which can lead to cement degradation and partial debonding under masticatory forces. Although this debonding does not necessarily result in crown detachment, it can cause microleakage and plaque accumulation, increasing inflammation in the surrounding tissue. Therefore, we should take all measures to reduce the risk of crown detachment. On one hand, it is recommended to appropriately surface treat the titanium Base; on the other hand, the choice of cementing system should be adapted to the selected ceramic restoration material. Furthermore, the structure of the titanium Base itself and its height may also play an important role in overall stability. Increasing the height of the restoration can create a larger bonding surface, and choosing longer and cylindrical titanium Bases may also help prevent restoration debonding.

For submucosal areas, titanium Base abutments with different gingival heights and shapes can be selected. A recent randomized controlled clinical trial suggested that longer gingival height abutments (≥2 mm) have a protective effect on marginal bone resorption, which may be particularly important in thin gingival cases. Additionally, narrow-neck or submucosal concave-shaped titanium Base abutments are currently clinically preferred as they show smaller marginal bone level changes and greater mucosal edge stability. Similarly, larger restoration angles (>30°) may increase the risk of peri-implantitis at the bone level. Therefore, when selecting titanium Base abutments, these factors should be considered. If the implant does not allow the use of straight screw abutments, angled screw abutments can be considered, but studies have pointed out that angled screw abutments, in addition to the risk of restoration fracture, may require more space for the tilted screw channel, which could reduce the height of the abutment, potentially leading to a decrease in the bonding surface and more frequent restoration debonding.
2.Customized CAD/CAM Abutments
Although titanium Base abutments have a wide range of clinical indications, and can even be used with angled screw abutments, they may not be the preferred choice in certain clinical scenarios, one aspect to consider being the crown-to-abutment ratio. Titanium Base short abutments supporting ultra-long implant crowns are more prone to bonding failure. In such cases, customized CAD-CAM titanium abutments may provide sufficient support, retention, and bonding for the restoration.
Customized CAD-CAM abutments can also be made of zirconia material. Initially, the use of all-zirconia abutments was proposed to improve aesthetics, but studies have pointed out that the abutment and restoration are prone to fracture, which may be related to the specific geometry and dimensions at the connection of the zirconia abutment. Additionally, some fractures were observed during abutment tightening, indicating that CAD-CAM zirconia abutments are sensitive to forces and may increase the risk of wear at the implant connection. Although personalized zirconia abutments are an effective solution for anterior aesthetic cases, their theoretical aesthetic advantage can be surpassed by titanium abutments, making their actual indications limited.
Implant-Supported Multi-Unit Fixed Restoration Abutment Selection
For multi-unit fixed restorations, titanium Base abutments can be used, but their selection mainly depends on the parallelism of the implants and the angulation of the restoration. In cases where the axes of multiple implants cannot be parallel, achieving passive screw-retained seating at the implant level is impossible. Using abutments with non-engagement or anti-rotational features may help solve the seating problem, thereby improving the fit of the restoration. However, some manufacturers only provide short tapered engagement titanium Bases, which may affect the stability of the cementation. Additionally, in vitro studies have shown that engaged abutments have higher mechanical stability compared to non-engaged abutments.
One solution is to use intermediate components at the abutment level for restoration, such as multi-unit abutments (MUA), which can compensate for some angle differences. A metal framework is designed according to the required restoration shape, and after fabricating veneers or all-ceramic crowns, it is directly screw-retained onto the MUA. Another solution is to use titanium Base, cement the entire or faceted zirconia restoration outside the mouth, and then screw-retain it onto the MUA. A common issue when using MUA is that it allows for reduced restoration screw torque, which may increase the risk of screw loosening.
Temporary Restoration Abutment Selection
When selecting temporary restoration abutments, titanium Base abutments remain the only solution for fully digital temporary restorations. However, a clinical issue encountered is the bonding stability problem of polymethyl methacrylate (PMMA) material on titanium Base. Nevertheless, using traditional temporary cylindrical titanium Base abutments is still the most reliable solution to avoid debonding.
Summary
For single implant restorations, it is recommended to use titanium Base abutments instead of traditional cast and customized metal or zirconia abutments, as titanium Base abutments can balance the mechanical stability of metal connections and the aesthetic effects of ceramics. For multi-unit bridge implant restorations, it is recommended to use tapered titanium Base abutments designed specifically for bridges to compensate for deviations in implant placement axes and angles. Although titanium Base abutments with different shapes and heights are currently available, customized titanium Base abutments can still play a role in certain clinical scenarios.




Comments (1)
Gema Houghtonsays:
07/26/2024 at 5:50 PMThanks for your help and for writing this post It’s been great