
Speakers: Shi Bing, Wu Min, West China Hospital of Sichuan University
This article is compiled from a lecture by Professor Shi Bing’s team, with Wu Min as the lead nurse, providing a detailed explanation on “How to Provide Early Care for Children with Cleft Lip and Palate.” The main topics covered include preoperative orthodontics, feeding challenges and strategies, cognitive development patterns and training, speech development characteristics and guidance, as well as preoperative preparation and perioperative care.
01 Preoperative Orthodontics
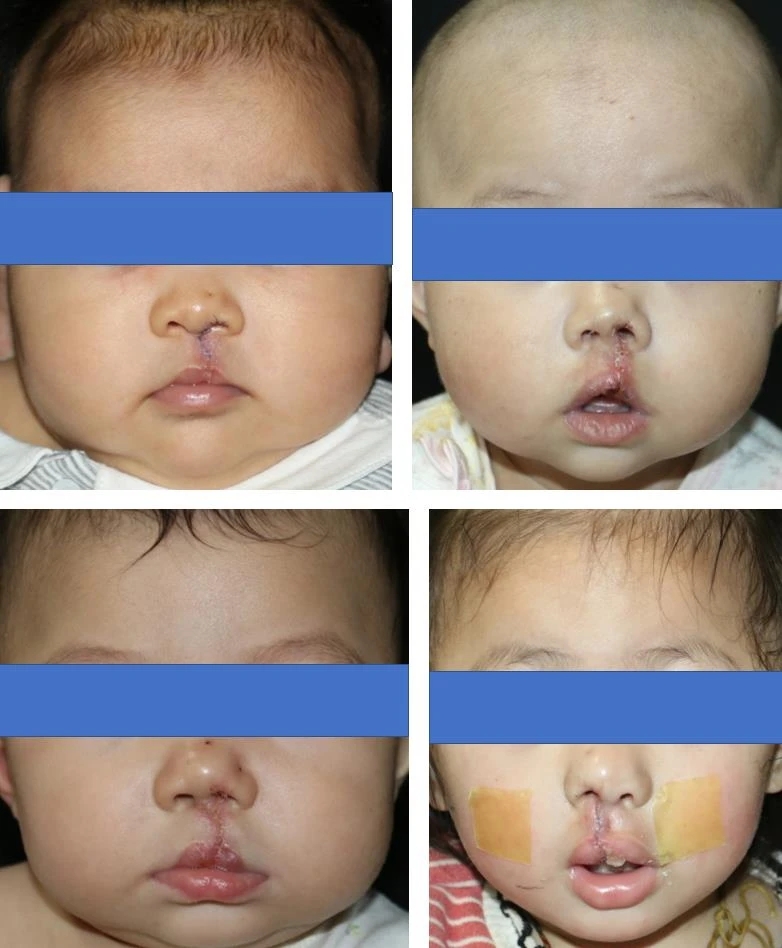
Children with cleft lip and palate often present with severe deformities of the lip, nose, and alveolar ridge, especially in cases of unilateral or bilateral complete cleft lip and palate. Without intervention, these deformities can worsen over time. The nasal cartilage of cleft lip and palate patients retains plasticity after birth, allowing orthodontic devices to correct deformities of the lip, nose, and alveolar ridge. This aids in establishing a normal tongue position and supports the growth of oral and maxillofacial soft and hard tissues, creating optimal conditions for surgical intervention and reducing surgical difficulty. Traditional preoperative orthodontic procedures are complex and resource-intensive. Since children continuously grow during this orthodontic process, they may need to visit the hospital for check-ups approximately 6-7 times from 7 days after birth until surgery, requiring repeated impressions and changes to the orthodontic device. Therefore, there is a need to explore improvements in preoperative orthodontic methods to allow parents to perform self-management, reducing medical expenses and travel burdens. We recommend a home-based self-service preoperative orthodontic approach for children with cleft lip, which can be completed during the initial consultation without frequent follow-ups. This method is simple for parents to learn and has high compliance rates. For children with complete cleft palates, an intraoral impression is taken at 7 days after birth, and further adjustments to the palatal plate can be made according to the orthodontic plan postoperatively, with another impression taken 2 weeks after lip repair. This greatly simplifies the preoperative orthodontic process. The steps for home-based self-service preoperative orthodontics are as follows: First, place one side of the orthodontic tape on the cheek of the cleft side. Using one hand’s index finger and thumb, gently push both cheeks towards the center to reduce the cleft gap. Then, place the other side of the tape on the non-cleft side, ensuring the middle part adheres to the lower edge of the upper lip, with the nose hook positioned at the affected side’s nasal dome. Tightening the nose hook should cause the skin at the edge of the nostril to whiten slightly. All these preoperative orthodontic supplies are single-use, easy to operate, and convenient for parents. The before-and-after effects of home-based preoperative orthodontics for a child with unilateral complete cleft lip and palate are shown in Figure 3.



02 Feeding Challenges, Strategies, and Precautions
- Feeding Challenges
The difficulties in feeding children with cleft lip and palate primarily stem from the cleft of the lip or palate, which creates an opening between the oral cavity and nasal cavity. This prevents the formation of a sealed space required to create the negative pressure necessary for effective sucking, leading to challenges such as effortful sucking, reduced intake, and prolonged feeding times. Additionally, the cleft palate alters muscle distribution and attachment, causing some muscles to overdevelop or underdevelop, which affects muscle tone and results in a retracted tongue, making it hard to effectively envelop the nipple during feeding. Lastly, children with cleft palates lack the ability to keep food or liquid out of the nasal cavity, making them particularly susceptible to choking. - Feeding Methods
Feeding methods primarily include breastfeeding, bottle feeding, and drop feeding.- Breastfeeding: Infants with cleft lip find breastfeeding relatively easier. The mother should clean and massage the breast to encourage milk flow, allowing the child to suck once the nipple is protruded. Parents of children with cleft lip can use their fingers to occlude the cleft area, assisting in lip closure; however, children with cleft palates struggle to create negative pressure due to the cleft.
- Bottle Feeding: Use a squeezable bottle with a soft latex nipple. The best choice is a specialized cleft lip and palate bottle equipped with an air vent and restrictor. This design allows the nipple to seal against the cleft palate, preventing collapse during sucking and ensuring smooth milk flow. The restrictor prevents backflow during sucking, requiring only light pressure from the tongue to release milk. For infants with weak sucking abilities, a squeezable bottle facilitates feeding. Post-surgery, spoon feeding can also be beneficial in avoiding pain at the surgical site.
- Drop Feeding: For younger infants or those post-surgery, drop feeding is convenient.
- Feeding Behavior Guidance
Feeding methods vary for different types of cleft lip and palate. For isolated cleft lip, although the oral and nasal cavities aren’t connected, air leakage may occur during sucking. Parents can use their fingertips to occlude the missing portion of the lip to create a sealed environment for effective feeding. For children with cleft palates, it’s advisable to use specialized cleft lip and palate bottles. If the cleft is too wide to facilitate feeding, preoperative orthodontics may be necessary to narrow it, promoting regular tongue movement and improving feeding outcomes. Proper nutrition during infancy is crucial, as a solid physical foundation is essential for the child’s surgical tolerance. - Post-Feeding Precautions
After feeding, it’s important to use the correct burping technique. Due to the immature development of the stomach and throat in infants, the stomach may be in an unstable horizontal position. As the stomach fills with milk and air, pressure may lead to spitting up or vomiting, even causing choking. Parents should promptly burp the baby post-feeding to expel gas. There are three recommended methods for burping:- Upright Position: Hold the baby upright against the shoulder, lightly tapping the back to encourage burping.
- Sitting Position: Have the baby sit on your lap facing you, supporting their head while gently tapping the back.
- Side-lying Position: Place the baby sideways across your lap, with the head slightly lower, supporting them with one hand while gently tapping their back. This position is more suitable for younger infants. If burping doesn’t occur after several attempts, start by gently rubbing the back before tapping.



03 Cognitive Development Patterns and Training
The psychological well-being of children with cleft lip and palate is increasingly recognized. The mother’s psychological stress and emotional variability have long-term impacts on these children, often resulting in limited mother-infant interactions. Children may show less engagement, with fewer signs of wanting to communicate, such as eye contact, physical touch, smiles, and verbal attempts. The attachment between mother and child is bidirectional, and mothers should be attentive to the emotional needs of their babies. Cognitive development in infants with cleft lip and palate does not show significant differences from typically developing children, primarily advancing through conditioned and unconditioned reflexes that enhance sensory and motor skills. When fostering cognitive abilities, family involvement is critical. Infants rely heavily on their immediate environment, so it is vital to guide parents in mastering feeding techniques. Family members should actively participate in the treatment sequence, understand the causes of cleft lip and palate, appropriate age for treatment, treatment plans, and the cosmetic outcomes post-treatment, while sharing successful case studies to help alleviate feelings of guilt, anxiety, and sadness. Additionally, parents are encouraged to learn about early childhood education to support their child’s development.
04 Speech Development Characteristics and Guidance
- Speech Development Characteristics in Cleft Palate Children
Parents are often most concerned about the clarity of their child’s speech. With advancements in clinical techniques, surgical intervention for cleft palate can now occur by age 1, aiming to reconstruct the necessary oral structures for normal phonation. However, children must adapt to substantial changes in their oral environment and learn to correctly utilize the repaired structures with proper articulation techniques. Typically developing children acquire speech skills sequentially, starting from semi-vowels to consonants. By 6-12 months, they begin to use a wider range of phonemes, often producing their first words around this time. In contrast, children with cleft palates may exhibit compensatory sounds early on, limited consonant variety, and predominantly produce nasally articulated sounds. Even after surgical intervention, compensatory articulation can persist, impacting later speech development. Nonetheless, children with cleft palates can express their intentions through gestures effectively. Those with limited verbal communication but clear gestural intent generally face lower risks of later speech deficits. - Early Family Speech Training Techniques for Cleft Palate Children
- Storytelling: Engaging storytelling using colorful picture books is an excellent way for parent-child interaction. Controlling the pace ensures the child can hear each sound clearly, while variations in tone can help convey the story’s emotional nuances, capturing the child’s attention.
- Syllable Stimulation: Regularly interacting with the child using varied pitches helps in auditory stimulation.
- Encouraging Verbalization: Parents should motivate their children to speak and guide them in mimicking sounds.
- Tongue Movement Training: This is a crucial part of post-surgical speech practice. Techniques include:
- Teaching the child to quickly tap the upper front teeth with their tongue to produce airflow sounds, practicing 10-20 times daily.
- Sliding the tongue from behind the upper front teeth to the lower front teeth to enhance tongue control, also 10-20 times daily.
- Rotating the tongue to lick the corners of the mouth and upper and lower lips, practicing 10-20 times daily.
- Oral Airflow Training: Teaching the child to blow air through their mouth to differentiate between oral and nasal airflow. This can include blowing on hot food, blowing into tissues, and practicing various blowing techniques.
- Phonetic Training: Emphasizing practice on the sounds /p/, /t/, and /k/ is recommended, as mastering these can facilitate learning other phonemes. Speech development is a gradual process, and consistency is key. Generally, by age 3, if the child can produce simple vowels and consonants, follow-up visits to the hospital’s speech clinic are advisable.
05 Preoperative Preparation and Perioperative Care
- Preoperative Preparation:
Prepare elbow restraints to help stabilize the child’s elbows and prevent touching the surgical site; have specialized cleft lip and palate bottles ready. Most importantly, parents should psychologically prepare themselves, as postoperative wound care, managing crying, and scar management will test their patience. - Optimal Surgical Timing:
The best time for surgery is between 3 to 6 months of age, with a general requirement for the child to weigh over 5-6 kg. - Postoperative Wound Care:
Maintaining a moist environment aids in wound cleaning and healing. Exudates can adhere to moist dressings, reducing scab formation and minimizing pain during dressing changes. Routine cleaning with 0.9% saline is recommended. In assessing the postoperative wound, dryness, absence of redness, swelling, purulent discharge, and no signs of ischemia are reassuring indicators. - Scar Management:
- Silicone Scar Treatments: These include silicone sheets and gels. Consistent use for 3-6 months post-surgery can help achieve the desired effects.
- Use of Lip Strips: During the healing and scar recovery process, muscle movement can widen scars. Applying low-allergy tape over the upper lip can reduce tension and minimize hypertrophic scarring. Continuous use for six months is advisable until complete softening of the scar occurs, with artificial skin used to protect the area.
- Scar Massage: Generally initiated one week post-stitch removal under non-inflamed conditions. For scar massage, use a gentle downward pressure with the index finger on hardened areas of the upper lip, avoiding rubbing. Each pressure session should last one minute and be repeated 6-8 times daily.
- Laser Scar Treatment: Currently a popular method for scar management. Early laser intervention can help prevent scarring.
- Postoperative Nasal Deformity Care:
Children will need to wear a “nasal splint” to shape the nostrils. Building on traditional nasal molds, Professor Shi Bing has designed a simplified nasal splint that only supports the nasal tip and columella, providing stability without additional anchoring devices. The splint attaches to the side of the columella without obstructing airflow, enhancing comfort and aesthetics, promoting prolonged wear. Daily use for 24 hours is recommended post-stitch removal, with results illustrated in Figure 11. - Follow-Up Observations:
Post-surgery, the physician should regularly monitor wound healing and scar recovery, providing parental guidance on scar care at various stages. For cleft palate children, follow-ups should focus on wound healing until stabilization is achieved.






Speaker Introduction
Professor Shi Bing

Professor Shi Bing is a second-level professor at Sichuan University, doctoral advisor, chief expert at West China Hospital of Stomatology, leader in scientific and technological innovation in Sichuan, and chair of the Sichuan Provincial Committee of Stomatology. He is a former chair of the Oral and Maxillofacial Surgery Committee of the Chinese Stomatological Association and the china Nation Cleft Lip and Palate Committee. He is also a member of the Cleft Lip and Palate Expert Committee of Operation Smile, and associate editor of the Ministry of Health’s textbook “Oral and Maxillofacial Surgery.” He has authored and translated numerous publications, including “Cleft Lip and Palate Reconstructive Surgery” and “Primary Cleft Lip and Palate Repair.” He is a recipient of multiple national grants and has published over 190 papers, with 90 included in SCI. His innovative theories and techniques, such as the new rotation advancement method and bilateral lip repair surgery, are widely applied in clinical practice. His primary research areas include the mechanisms of congenital cleft lip and palate, growth and development patterns, and new clinical treatment techniques.
Wu Min, Lead Nurse

Wu Min is a supervising nurse and speech therapist in the Cleft Lip and Palate Department at West China Hospital of Stomatology, with expertise in wound care. She has published over 20 academic papers in recognized domestic and international journals, including the “West China Journal of Stomatology” and the “International Journal of Oral Medicine.” She is a co-author of the book “Nursing Care for Cleft Lip and Palate” and has participated in numerous charitable activities for children with cleft lip and palate.




Leave a Reply