
Overview
When patients experience severe wear of the entire dentition, enamel hypoplasia, or radiation caries after radiotherapy, the occlusal vertical dimension may decrease, necessitating an increase in the patient’s occlusal vertical dimension and occlusal reconstruction.
With the continuous deepening of research by scholars at home and abroad, the current field of occlusal reconstruction incorporates the study of the musculature of the maxillofacial region and the temporomandibular joint into the scope of occlusal reconstruction of the stomatognathic system, considering the overall aesthetics of the teeth, their form, function, and the esthetics of the maxillofacial region. Therefore, modern occlusal reconstruction theory mainly includes four main aspects: mandibular position, vertical distance, occlusal plane, and dynamic guidance and static occlusion.
Digital Application Process
(I) Determining the Mandibular Position
Finding a comfortable and stable mandibular position is the first step in occlusal reconstruction treatment. Subsequent designs for vertical distance, occlusal plane, and dynamic/static occlusal type are based on this position, making the mandibular position the most important factor in occlusal reconstruction. Currently, the latest definition of centric relation is as follows:
(1) Clinically unrelated to tooth contact;
(2) The articular eminence is in the most forward and upward position, directly facing the posterosuperior slope of the articular eminence;
(3) At this position, the mandible only performs pure rotation;
(4) In a comfortable physiological state, the mandible can start forward, sideways, and upward movement from this position;
(5) A repeatable reference position.
Finding and determining the mandibular position manually is the first step in traditional occlusal reconstruction, including the use of the bimanual guidance method and the chin point guidance method. However, these methods require extensive clinical training to achieve good repeatability and accuracy, making occlusal reconstruction a highly technique-sensitive medical procedure that is not conducive to mastering and popularizing.
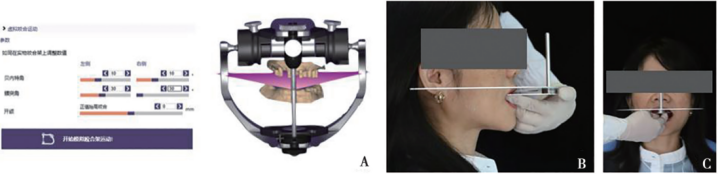
The introduction of digital technology is expected to improve this situation. The electronic facebow, also known as a motion facebow, is an important tool in the digital clinical process for finding and determining the mandibular position in occlusal reconstruction.
The electronic facebow, as opposed to the traditional mechanical facebow, can not only transfer the jaw relationship of a specific reference plane, such as the orbitomeatal or nasion-ear plane, but can also record the personalized mandibular movement trajectory and determine the centric relation through data analysis.
After determining the centric relation, bite registration with silicone rubber can be used to record the patient’s bite relationship at this time and combined with the mandibular movement data obtained from the electronic facebow (e.g., lateral condylar guidance inclination, protrusive condylar guidance inclination, etc.) for subsequent articulator operations. The horizontal and vertical errors of the electronic facebow are currently within approximately 2 mm, and the angular error is approximately 2°, meeting clinical accuracy requirements.


(II) Determining the Vertical Dimension
The vertical dimension refers to the vertical height from the nasion to the menton during natural occlusion and is also known as the occlusal vertical dimension. For occlusal reconstruction, it is necessary to first determine whether the existing vertical height is within the physiological adaptation range. If it is not within this range, a decision needs to be made to either increase or decrease the existing vertical dimension.
In cases where there is obvious wear of the dental arch or significant loss of posterior teeth that serve as support, there is likely a decrease in the vertical dimension, and it is advisable to raise the occlusal height appropriately for subsequent occlusal reconstruction. It is particularly important to note that for patients requiring adjustments to the vertical dimension, reversible operations must be performed before any irreversible operations to verify the safety and correctness of the occlusal changes, such as using bite raising appliances or diagnostic bite veneers. Traditional methods for determining the vertical dimension include facial observation, evaluation of existing old dentures, and past facial profile assessments.
In addition to the above methods, the digital era has introduced the combination of big data prediction and lateral cephalometric radiographs for evaluating the vertical distance. The lateral cephalometric radiograph can be used to measure the lower face height, and, combined with a large amount of population vertical distance data, can predict a safe space for vertical distance adjustment for the patient. However, to date, there is no single reliable method for determining the vertical dimension, so it is necessary to use a variety of methods for comprehensive assessment in clinical practice.


(III) Determining the Occlusal Plane
The occlusal plane has multiple definitions in the field of dentistry. The currently widely accepted definition refers to the imaginary plane constructed from the mesial contact point of the maxillary central incisors to the buccal cusp tip of the first maxillary molars.
For occlusal reconstruction patients, it is necessary to confirm whether the existing occlusal plane meets the requirements of physiological functional movement before reconstruction. If the occlusal plane meets the following requirements, occlusal reconstruction can be carried out based on this occlusal plane:
– From the coronal view, the occlusal plane should be parallel to the line connecting the pupils on both sides;
– From the sagittal view, the occlusal plane should be parallel to the nasion-ear plane;
– Place the occlusal frame on the model and observe whether the occlusal plane evenly divides the maxillary and mandibular occlusal space.
The coordination between the Spee curve, the Wilson curve, and the occlusal plane should also be considered.
By using a virtual occlusal frame, it is possible to observe whether the occlusal plane meets the above requirements and to design the Spee curve and Wilson curve based on the personalized occlusal parameters obtained from the electronic facebow. Additionally, a bite plane can be used for further verification outside the mouth.

(IV) Dynamic Guidance and Static Occlusion
When the mandible is in functional movement, the teeth play a certain guiding role, as evidenced by protrusive and lateral guidance. Protrusive guidance is a protective mechanism of mandibular movement related to the function surfaces of the anterior teeth and some cuspid teeth.
During protrusive movement of the mandible, the anterior mandibular teeth follow the guiding form of the lingual surfaces of the maxillary anterior teeth and some cuspid teeth, resulting in natural separation of the posterior teeth to avoid interference with posterior tooth movement and wearing of the articular eminence.
Lateral guidance is also a protective mechanism of mandibular movement. When the mandible moves laterally, the working side guide separates the non-working side occlusion to avoid interference with the non-working side teeth.
Static occlusion refers to the way the upper and lower teeth make contact during occlusion.
Both dynamic guidance and static occlusion involve the coordination between tooth form and personalized occlusal parameters (e.g., protrusive condylar guidance inclination, lateral condylar guidance inclination, immediate lateral shift, etc.).
Using digital methods, it is possible to digitally reproduce the individualized mandibular functional movement trajectory of the patient based on the personalized occlusal parameters obtained from the electronic facebow and the virtual occlusal frame. This can be used to guide the design of tooth form and determine dynamic guidance and static occlusion. Before the final restoration is made using CAD/CAM, virtual occlusal adjustments can also be made.
Multimodal Data Fusion Application
The digital process described above has brought convenience to clinical work, but the data is dispersed and can only be assessed one by one. The use of multimodal data fusion technology greatly makes up for this deficiency.
The following is an example of the establishment of a four-dimensional virtual dental patient based on multimodal medical data fusion and the method of increasing the vertical distance to achieve occlusal reconstruction. The visual, operable fusion object enables simultaneous consideration of occlusal reconstruction, repair space, anterior aesthetic, occlusion, and the safe position of the articular eminence in the joint fossa of the stomatognathic system.
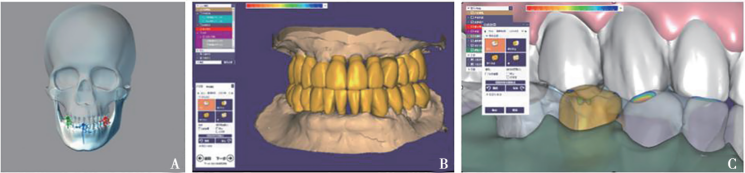
First, intraoral scanning is used to obtain a three-dimensional surface model of the original dental arch and the static maximum intercuspation occlusion relationship, saved as an STL format, known as STL-dental arch. This data is easy to obtain, low in cost, and allows for a relatively intuitive analysis of the static occlusal situation of the dental arch.

Next, the patient’s cone-beam computed tomography (CBCT) data with a large field of view is obtained to measure the vertical dimension. By adjusting the ideal surface grayscale threshold value and manually optimizing the contour of the articular eminence, the surface of the articular eminence can be automatically reconstructed, establishing three-dimensional surface models of the maxilla and mandible and saving them as STL-maxilla and STL-mandible to lay the foundation for the fusion of intraoral scanning and maxillofacial three-dimensional surface models.

The STL-dental arch and STL-maxilla/mandible data are imported into the software for registration and segmentation to ensure that the surface model of the maxilla is in the same spatial coordinate system as the dental arch and to obtain the processed maxillary and mandibular surface models, combining the advantages of the CBCT of the maxilla and the high-precision intraoral scan data.

The matched maxillary and dental arch data are imported into the optical sensor-based mandibular movement analysis system, and the headset optical signal receiver is worn on the patient’s head to locate the maxillary position, while the mandibular optical receiver is placed on the buccal side of the mandibular dental arch. The optical signal receiver is fixed using light-curing fluid resin to record the mandibular movement trajectory without affecting occlusion, avoiding interference with occlusion, and recording the mandibular movement trajectory.

The fusion of extraoral facial scanning data can be combined with the processed maxillary and dental arch data. After the fusion of the “surface” and “bone,” the final four-dimensional virtual dental patient is obtained.

After the creation of the four-dimensional virtual dental patient, it is possible to observe and analyze static occlusion, dynamic guidance, occlusal area, and the displacement trajectory and range of the articular eminence movement process from the sagittal, coronal, and horizontal planes at any angle. This allows for the visualization and manipulation of the four-dimensional virtual dental patient to find new centric positions and further carry out clinical occlusal reconstruction work.

Conclusion
Occlusal reconstruction is a highly technique-sensitive clinical procedure that involves not only dental tissues but also masticatory muscles and the temporomandibular joint. Occlusal reconstruction should not only consider how to rebuild the dental form but should also comprehensively consider how to rebuild the personalized and comfortable stomatognathic system.
The key to successful occlusal reconstruction lies in systematically and standardly considering mandibular position, vertical distance, occlusal plane, dynamic guidance, and static occlusion, and avoiding complications of occlusal reconstruction. With the continuous development of digitization, many digital-assisted devices have emerged in the field of occlusal reconstruction, constantly improving and promoting the development of occlusal reconstruction towards precision and personalization.
The digital occlusal reconstruction plan presented today has the advantages of visualization, personalization, practicality, and strong openness. However, caution must be exercised to avoid neglecting the importance of clinical processes due to the assistance of digital equipment. Additionally, digital technology still has some limitations, such as the high cost of digital equipment, and the need for medical professionals to flexibly adjust digital occlusal reconstruction steps according to specific patient conditions.
Reference.
[1] 何凯讯,张思慧,陈江.数字化咬合重建的流程管理[J].口腔医学,2021,41(03):193 -197+230.DOI:10.13591/j.cnki.kqyx.2021.03.001.
[2] 孙欣荣,冯玥,刘伟才.多模态数据融合的可视化技术在咬合重建中的应用[J].华西口腔医学杂志,2022,40(04):468-475.
[3] Talaat WM,Adel OI,Al Bayatti S.Prevalence of temporomandib-ular disorders discovered incidentally during routine dental exami-nation using the Research Diagnostic Criteria for Temporomandibular Disorders [J] .Oral Surg Oral Med Oral Pathol Oral Radiol,2018,125 ( 3) : 250-259.
[4] Janal MN,Raphael KG,Nayak S,et al.Prevalence of myofascial temporomandibular disorder in US community women [J] .J Oral Rehabil,2008,35 ( 11) : 801-809.
[5] Wieckiewicz M , Grychowska N , Wojciechowski K ,et al.
Prevalence and correlation between TMD based on RDC / TMD di- agnoses ,oral parafunctions and psychoemotional stress in Polish University students [J] .Biomed Res Int,2014,2014 : 472346.
[6] 林潇,梁超,岳新新 ,等.数字化技术辅助无牙颌种植固定修复咬合重建的临床应用初探 [J] .中华口腔医学杂志,2020, 55 ( 11) : 891-896.
[7] Theglossary of prosthodontic terms : ninth edition [J] .J ProsthetDent,2017,117 ( 5S) : e1-e105.
[8] Zhang SH,He KX ,Lin CJ,et al.Efficacy of occlusal splints in the treatment of temporomandibular disorders : a systematic review of randomized controlled trials [J] .Acta Odontol Scand,2020,78 ( 8) : 580-589.
[9] Li B, Li XQ, Yi XZ. Effect of severe dental attrition on facial height[J]. J Modern Stomatol, 2007, 21(3): 307- 308.
[10] Yang F, Li Z, Wang FL, et al. Six-stage practical treat‐ ment principle of occlusal reconstruction[J]. Chin J Pract Stomatol, 2021, 14(5): 621-628.
[11] Liu YP. Restoration of occlusionn height before fixed prosthesis[J]. J Pract Med, 2013, 29(9): 1490- 1491.
[12] Du X, Qu F, Liu WC. Establishment of a three-dimen ‐ sional virtual dental patient and its application in esthet‐ ic restoration[J]. Int J Stomatol, 2018, 45(6): 695-702.




Leave a Reply