
This case was included in the “Spark Plan” 2023 Best Clinical Practice in Dentistry
Authors: Liu Hengyan, Liu Yuchen, Li Kangjie, Zhong Sheng, Bai Shizhu, Fang Ming
Department of Prosthodontics, the Third Affiliated Hospital of Air Force Medical University
01 Patient’s Basic Information and Diagnosis
01 Elderly male patient
Chief complaint: Lower anterior teeth have been loose for 3 months, affecting chewing, and requires restoration.
Medical history: Multiple loose teeth and tooth loss in recent years, received periodontal basic treatment in the periodontal department; three teeth have been restored with implants.
Past medical history: No significant medical history or family history.
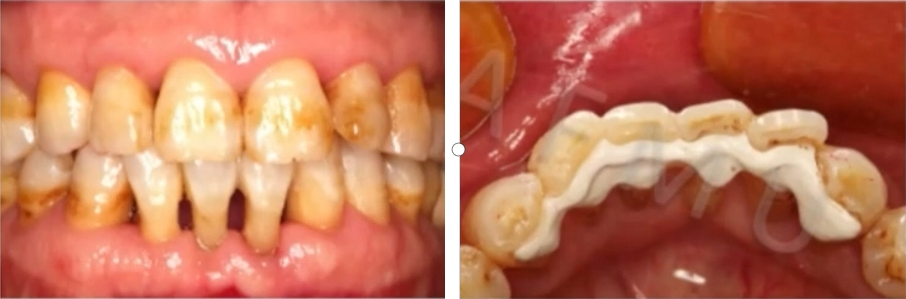
Oral examination: Missing teeth in the posterior region (16, 17, 36, 37, 47), with implants in 16, 36, and 37; lower central incisor has Grade III mobility, while the lower lateral incisor is stable (see Figure 1).
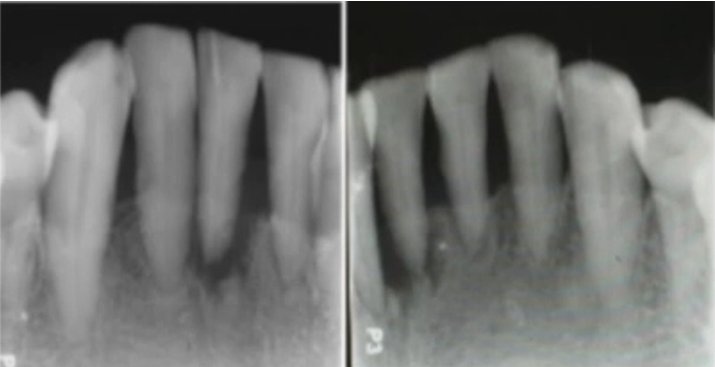
Radiographic examination: Periapical radiographs show bone resorption of Grade II-III around teeth 32-42, root fracture at 1/3 of tooth 41, and extensive periodontal shadow (see Figure 2).
Diagnosis: Root fracture of tooth 41, Stage IV periodontitis, and dental arch defect.

02 Design and Consideration of Treatment Plan
Treatment plan: Extract tooth 41, periodontal treatment, and restoration of tooth 41 (17 and 47 not restored for now).
Choice of restoration plan: For the severe periodontitis patient with missing lower anterior teeth, implant restoration is difficult due to the small gap and high aesthetic risk, and it cannot address the patient’s loose teeth issue. Removable prostheses create a strong foreign body sensation and are inconvenient to use, and the patient rejects them. Conventional fixed prostheses require significant tooth preparation and are difficult to remove for future modification. Considering that only one tooth needs restoration and the lower incisors only have mild coverage, the option of minimally invasive restoration with a periodontal splint was chosen. This approach not only restores the missing tooth but also redistributes the occlusal forces through splinting, promoting periodontal tissue healing and improving chewing efficiency.
Choice of material: Ligature wire and composite resin splints are only suitable for temporary use. Currently, the most commonly used in clinical practice is the fiber-reinforced composite resin splint, but it is prone to discoloration, plaque accumulation, resin delamination, and secondary caries, so it is mostly used for short- to medium-term purposes. Metal splints with better mechanical properties have the advantages of high strength, low foreign body sensation, and reduced risk of plaque accumulation and can be digitally fabricated. However, the metal bonding performance is limited, necessitating the addition of auxiliary mechanical fixation, increasing tooth preparation and the risk of secondary caries.
Literature review indicates that using polyetheretherketone (PEEK) for periodontal splints can achieve good fixation effects, but lacks long-term clinical efficacy observation. PEEK is a high-performance thermoplastic polymer, with polyetheretherketone (PEEK) being the most commonly used. Due to its excellent mechanical properties, good biocompatibility, and wear resistance, it is increasingly used as a medical implant material and is widely applied in the field of dentistry. Compared to other methods, the advantages of PEEK periodontal splints lie in their high mechanical strength, thin thickness (0.7-1.0 mm), which allows for minimally invasive or non-invasive tooth preparation, reduced foreign body sensation after restoration, and high bending strength, allowing for elastic fixation of the loose teeth, which is conducive to periodontal tissue recovery. In addition, the entire process can be digitized, with short chairside operation time and low technical sensitivity.
Choice of bridge fabrication method: The current methods for digital fabrication include casting, CNC machining, and 3D printing. The production of the periodontal splint does not involve complex internal structures and requires high surface quality. Therefore, in this case, CNC machining was chosen to fabricate the PEEK splint. When considering the bridge fabrication method, four alternative options were considered: prefabricated resin teeth, 3D printed resin teeth, integrated PEEK splint bridge with veneered resin, and autogenous teeth. Although it is slightly cumbersome to use autogenous teeth for bridge fabrication, it provides the best aesthetic results, so this option was chosen for this case.
Timing of periodontal splint insertion: Literature review indicates that the timing of periodontal splint insertion directly affects the treatment effect. Inserting the splint before subgingival scaling or periodontal surgery can reduce periodontal trauma during scaling and achieve better periodontal treatment results. Inserting the splint after periodontal treatment allows for better assessment of the splint’s indication and clear treatment vision.
In this case, the patient’s bone resorption in the incisor region has reached Grade II-III, and there are several issues: after periodontal treatment, the mobility of the teeth cannot be significantly improved; due to root fracture of tooth 41, there is an aesthetic defect after extraction; for the patient, severe tooth mobility seriously affects daily chewing function and comfort. To address these problems as early as possible, the decision was made to insert the splint before periodontal treatment.
Treatment process:
① Intraoral digital scanning; ② Gingival curettage and sandblasting; ③ Extraction of tooth 41; ④ Fabrication of PEEK periodontal splint and bonding guide; ⑤ Preparation of a bridge using the extracted natural tooth 41; ⑥ Bonding under the guidance of the guide; ⑦ Subgingival scaling and surgical treatment after restoration, followed by regular periodontal maintenance.
03 Treatment Process
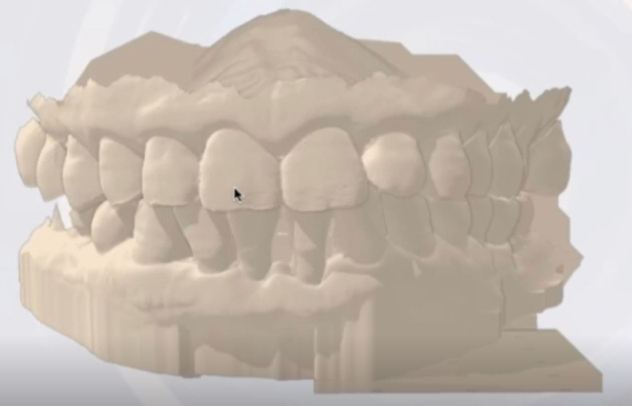
Before tooth extraction, the patient underwent intraoral scanning to produce a digital model (see Figure 3). It is important to ensure that the scanning range covers the proximal surfaces of the patient’s abutment teeth, as these surfaces need to be partially encapsulated during the design of the periodontal splint. After the patient’s oral hygiene, tooth 41 was extracted (see Figure 4). Computer-aided design was used to create a PEEK periodontal splint that matches the curvature of the tissue surface and lingual surface of the incisor, with the margin located at the gingival margin, not covering the interdental space, and not covering the incisal edge to avoid altering the patient’s anterior teeth occlusion (see Figure 5). The design range of the periodontal splint was 43–33, with a thickness of 0.7 mm.

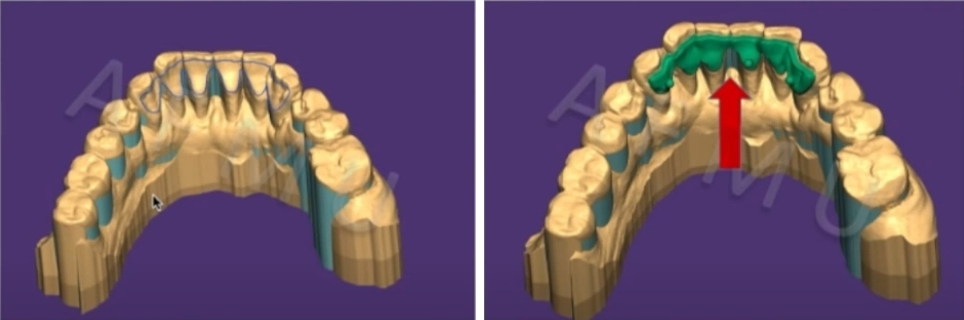
When fixing the splint to stabilize the loose teeth, dentists often manually press the splint towards the lip, which may cause slight movement of the loose teeth towards the lip, resulting in reduced adaptation between the splint and the lingual surface of the abutment teeth, affecting the durability of the splint. Therefore, a precision bonding guide was designed to aid in the precise bonding of the splint. The PEEK periodontal splint made by CNC machining and the 3D printed resin guide are shown in Figure 6. Guide 1 prevents changes in the original occlusal relationship of the patient, avoids tooth movement during bonding, and facilitates the formation of a uniform layer of adhesive; Guide 2 connects to the prominences on the polished surface of the splint and is used for holding the splint during bonding. The fixation rod of Guide 2 is connected to Guide 1 (see Figure 7). First, Guide 1 was positioned in the mouth, then the splint was assembled with Guide 2, and after assembly, the guide was positioned in the mouth. The assembly of Guide 1 and Guide 2 ensures precise positioning of the PEEK splint in the mouth.
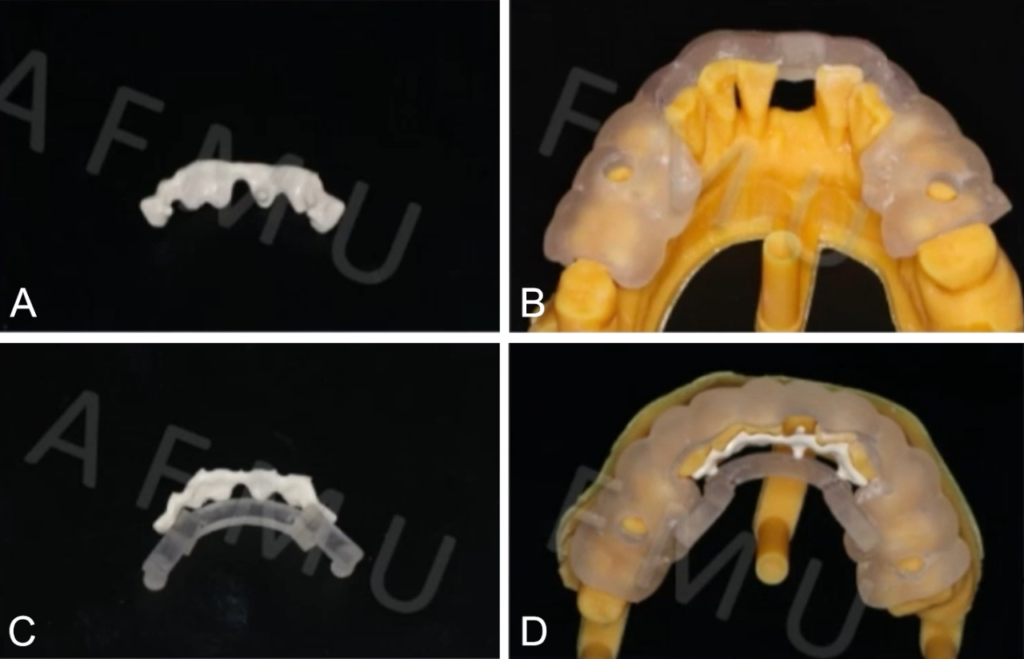
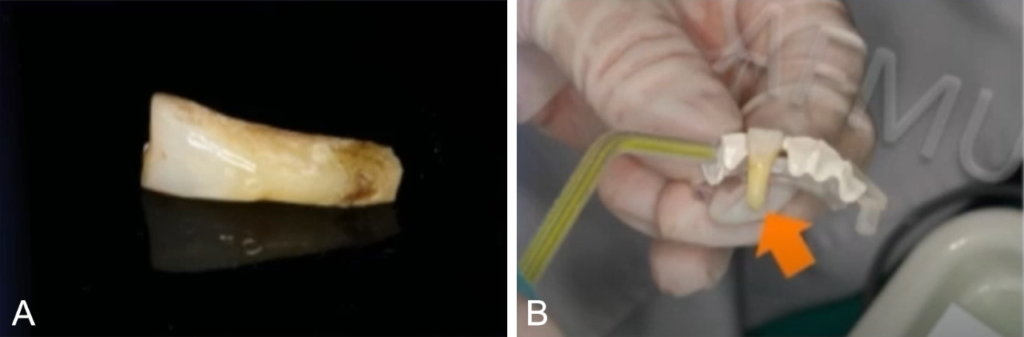
Figure 7: A: Trimmed tooth 41; B: Bridge fabricated using tooth 41
The periodontal splint primarily relies on adhesive fixation, and the adhesive performance is a key factor that affects the long-term efficacy of PEEK periodontal splints and whether they can be widely applied. Due to the biological inertness and low surface energy of PEEK materials, they require acid etching or sandblasting combined with adhesive primers to improve bonding performance. Therefore, the tissue surface of the splint was sandblasted, acid-etched, and coated with adhesive primer to form a chemical bond, thereby improving bonding performance. The lingual surface of the lower anterior teeth was not prepared, and after sandblasting and acid etching, a universal adhesive was applied, followed by bonding using dual-curing resin cement under the guide’s guidance, fine occlusal adjustment, and sequential polishing.
04 Treatment Results and Follow-up
The immediate postoperative intraoral image shows that good aesthetic results were achieved using the natural tooth as a bridge, with a similar appearance to before treatment (see Figure 8). The interdental space remains open, which is beneficial for self-cleaning by the patient and for later periodontal maintenance.

Three months after restoration, due to the patient’s habit of biting hard objects, partial debonding occurred at the 31 and 32 splinted teeth (see Figure 9). At the debonded sites, after removing the adhesive with a polishing bur and increasing the bonding space, re-bonding with dual-curing resin cement still resulted in good restoration. The patient rated the function and aesthetics of the periodontal splint highly but reported a strong foreign body sensation. Six months after restoration, the patient was satisfied with the restoration and reported a reduction in the foreign body sensation after a few months (see Figure 10).

Thirteen months after restoration, the splint at teeth 31 and 32 debonded again, and after re-bonding, the occlusion was adjusted (see Figure 11). The debonding of teeth 31 and 32 may be related to the patient’s habit of biting hard objects and the lateral tipping of tooth 32 and Grade III mobility of tooth 31.

Thirty-two months after restoration, the splint showed no debonding or fracture, and there was no significant change in the periapical radiograph compared to before (see Figure 12). The comparison of the periapical radiograph before restoration and 32 months after restoration shows slight bone resorption at the extraction site of tooth 41, while the bone level of the other abutment teeth is relatively stable, and a bone trabecular pattern has formed on the labial side of tooth 42, indicating stable periodontal bone status.

05 Current Research Status of PEEK Periodontal Splints
Clinical studies on PEEK periodontal splints have been registered and completed in 8 cases using clinical trials. Among these, 3 cases experienced partial debonding of the splint, and 1 case experienced debonding of the autogenous tooth used for restoration, with no occurrences of splint fracture, loosening of teeth, tooth loss, fracture of the prosthetic or natural teeth, or other complications. For patients with debonding, it was found that they tended to bite hard objects with their anterior teeth. Therefore, it is important to emphasize to patients wearing splints to avoid using their anterior teeth to bite hard objects. In follow-up observations, it was found that teeth with twisting or tilting and teeth with high mobility were more prone to debonding, but after re-bonding, good restoration results were still achieved.
Further observation evaluated the impact of loose teeth before and after insertion of the periodontal splint on oral health. Statistical analysis showed a significant improvement in the quality of life of patients 3 months after the periodontal splint restoration, but due to the limited sample size, more cases are needed to confirm the accuracy of the research results.
06 Summary
In this case, the application of intraoral digital scanning technology combined with CNC machining and 3D printing technology allowed for the entire process of producing digital PEEK periodontal splints from model collection to personalized design and computer-aided manufacturing. This approach overcomes the issue of tooth movement during traditional impression-taking operations, improves the quality of the impression, the accuracy of splint production, and the aesthetic results after restoration, and enhances patient comfort, while reducing technical sensitivity and improving work efficiency. The resin guides used in this case ensure the precise positioning of the splint during bonding, avoiding tooth movement during the bonding process, making the operation more convenient, and conducive to the formation of a uniform layer of adhesive and improving the long-term restoration effect.
Advantages of PEEK material in the fabrication of periodontal splints:
- High tensile and bending strength of the material, allowing for minimally invasive or non-invasive tooth preparation;
- PEEK material can provide the periodontal splint with a certain degree of elasticity, preserving the normal physiological mobility of the abutment teeth after bonding, promoting periodontal tissue repair;
- It can simultaneously restore the missing teeth within the splint, whether using artificial teeth, natural teeth, or veneered resin;
- The material’s low surface energy makes it less prone to plaque adhesion, reducing the risk of secondary caries after restoration, especially beneficial for periodontal disease patients;
- The entire digital manufacturing process reduces chairside operation time and improves work efficiency;
- The material does not pose a risk of allergic reaction, does not affect magnetic resonance imaging, and is suitable for various populations.
Key aspects of PEEK periodontal splint restoration:
Strictly adhere to the indications, design the splint reasonably, use guides to assist bonding, follow standard bonding procedures, and make precise adjustments
Indications for digital PEEK periodontal splints:
- Suitable for individual teeth with mild mobility in the anterior region, bone resorption ≤ 2/3 of the root length, and ≤2 missing teeth in the anterior region, with sufficient abutment teeth for fixing the loose teeth, adequate healthy enamel on the abutment teeth, and no severe crowding or tilting of the dental arch;
- No missing teeth in the posterior region, or the missing teeth in the posterior region can be restored with implants;
- More suitable for patients with Stage II-III periodontitis, with inflammation under control and good oral hygiene before restoration;
- Not applicable to bruxism or severe clenching patients, patients with no organic lesions in the temporomandibular joint, and no limitations in mouth opening. Better restoration and long-term outcomes are achieved for short-span splints.
07 Expert Review
Associate Professor Wang Fu: Tooth loss caused by periodontal disease is a common clinical problem, and restorative treatment must consider both the restoration of missing teeth and the preservation of remaining teeth. The restoration of periodontal splints is a common treatment for periodontal disease, but in traditional clinical treatment, the splint is manually adhered by the dentist, which may lead to the splint having a locally excessive adhesive layer due to slight movement of the loose teeth, affecting the durability of the periodontal splint. Avoiding minor tooth movement during bonding and other clinical operations is a clinical challenge.
In this case, the advantages of digital technology and bonding technology were fully utilized, especially the design and fabrication of personalized adhesive guide plates, which ensure the precise positioning of the periodontal splint during bonding, improving the accuracy of the restoration effect, reducing the difficulty of the operation, and ultimately achieving the desired restoration results. It is hoped that further clinical research will provide more validation and optimization of the restoration effect of this technology.
Digital technology has gradually become the mainstream technology in clinical diagnosis and treatment of dental restoration. Precision and convenience are the main development trends in the future. Hopefully, there will be more opportunities to work with domestic peers to create the future of digital restoration together.
Contributors:

Liu Hengyan, MD
Liu Hengyan, a master’s student in Prosthodontics at the Third Affiliated Hospital of Air Force Medical University, under the guidance of Associate Professor Fang Ming. A specialist member of the Prosthodontics Committee of the Chinese Stomatological Association. As the main applicant, she has applied for 1 invention patent, obtained 2 utility model patents, published 3 SCI papers, 3 Chinese core papers, and contributed to one monograph.

Associate Professor Wang Fu
Wang Fu, Deputy Director and Associate Professor of the Department of Prosthodontics at the Third Affiliated Hospital of Air Force Medical University, a doctoral tutor. Visiting scholar at the Tokyo Medical and Dental University, Japan. Currently serving as the Deputy Director of the Prosthodontics Committee of the Shaanxi Stomatological Association; a member of the Prosthodontics Committee and Aesthetics Committee of the Chinese Stomatological Association; and the first young lecturer of the Aesthetics Committee of the Chinese Stomatological Association. He is a core member of the National and Shaanxi Provincial First-Class Undergraduate Courses and has won the first prize for teaching achievements in higher education in Shaanxi Province. He has long been committed to the design and optimization of all-ceramic dental materials. He has presided over 4 national and provincial research projects and has published more than 30 SCI papers with a highest single paper citation of over 180 times. He has won the first prize for scientific and technological progress from the Ministry of Education, the first prize for scientific and technological progress in Shaanxi Province, and the special prize for scientific and technological research achievements in higher education in Shaanxi Province.
This translation aims to accurately convey the content of the original document.




Leave a Reply