
1.Types of Implant Fractures
The binary clinical classification method for implant fractures proposed by Li Yi et al. includes two dimensions: the morphology of implant fracture (F) and the degree of bone defect (D).
Implant fractures are classified into vertical fractures at the neck (F1), horizontal fractures at the neck (the fracture level is located at the neck of the implant, F2), and deep horizontal fractures (the fracture level is located near the bottom of the screw channel, F3).
The degree of bone defect is divided into no obvious bone resorption or narrow intra-bone pockets (D1), four-walled cup-shaped bone defects (D2), and cup-shaped defects accompanied by buccal/lingual bone plate defects (D3).
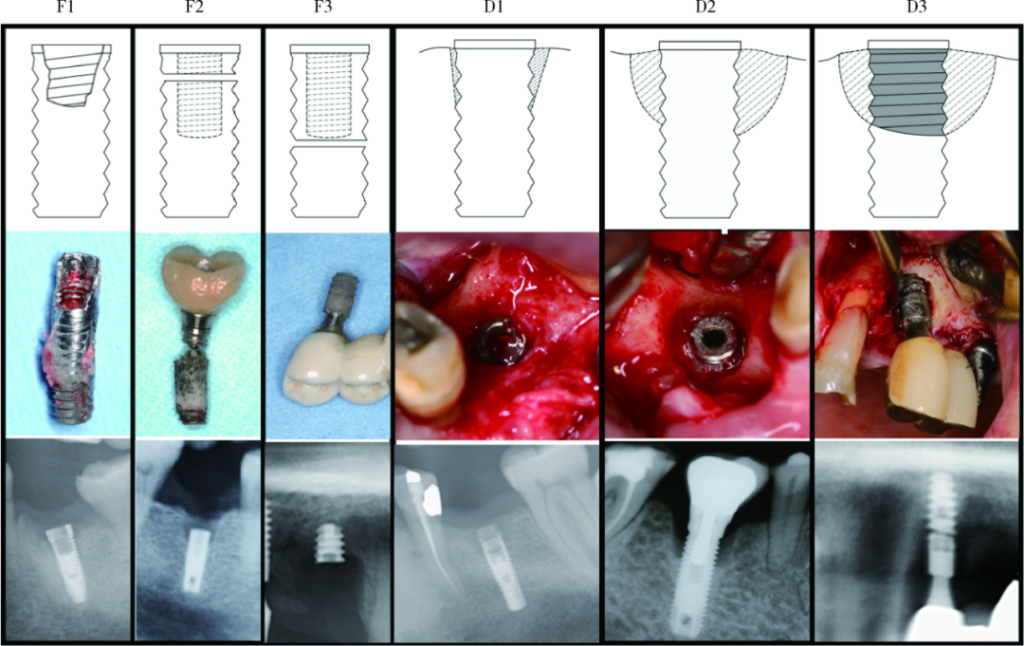
From left to right: F1, vertical fracture at the implant neck; F2, horizontal fracture at the implant neck; F3, deep horizontal fracture of the implant; D1, no bone defect or narrow sub-bone defect; D2, wide four-walled bone defect or cup-shaped defect; D3, wide three-walled or two-walled defect.
From top to bottom: charts, clinical photos, and periapical X-rays.
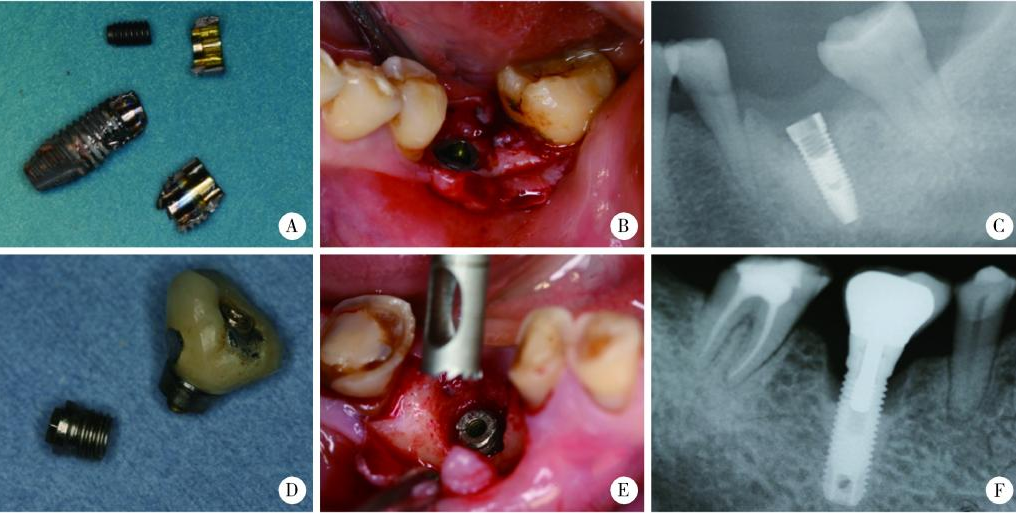
A, clinical photo of the fracture morphology of the implant of type F1D1; B, clinical photo of the bone defect of type F1D1; C, periapical film of type F1D1; D, clinical photo of the fracture morphology of the implant of type F2D2; E, clinical photo of the bone defect of type F2D2; F, periapical X-ray film of type F2D2.
2.Relationship between Implant Fractures and Bone Resorption
Regarding the relationship between implant fractures and surrounding bone resorption, there are currently two views:
One view holds that excessive implant loading may lead to primary marginal bone resorption (mostly cup-shaped bone resorption). As the supporting tissues of the implant decrease, the lever arm above the osseointegration increases, generating a greater leverage force. When bone resorption reaches the weak area inside the central screw channel, the implant is prone to horizontal fractures.
The other view is that factors such as excessive implant loading, poor seating of the prosthesis, andUndesirable restoration design can lead to primary implant fractures. The integrity of the soft tissue seal is disrupted, which in turn causes secondary bone resorption (mostly narrow and localized bone resorption).
Studies have found that the vertical fracture at the implant neck (F1) is significantly associated with the narrow and localized bone resorption around the implant (D1), and the horizontal fracture at the implant neck (F2) is significantly associated with the cup-shaped bone resorption around the implant (D2). These results confirm the rationality of the above two views.
It suggests that good implant structure design, prosthesis design, and load control may prevent the occurrence of F1D1 type implant fractures, while preventing peri-implantitis and soft and hard tissue defects may reduce the occurrence of F2D2 type implant fractures.
3.Risk Factors for Implant Fractures
– Implant Diameter
Sánchez-Pérez et al. believe that an implant diameter of less than 4.0 mm is a risk factor for implant fractures.
Srimaneepong et al.’s research on the torsional strength, ductility, and fracture characteristics of titanium and titanium alloys showed that the fracture resistance of a 5-mm-diameter implant is three times that of a 3.75-mm-diameter implant, and the fracture resistance of a 4-mm-diameter implant is also 30% higher than that of a 3.75-mm-diameter implant.
Chrcanovic et al. analyzed the relevant factors of 44 fractured implants and found that for every 1-mm increase in implant length, the fracture rate increased by 22.3%; for every 1-mm increase in implant diameter, the fracture rate decreased by 96.9%.
– Implant Connection Methods
Implant connection methods can be divided into internal connection and external connection. The internal connection method has a weak area in the anti-rotation groove at the implant neck, and this weak area may also become a site prone to fractures, which is more obvious in narrow-diameter implants.
The horizontal plane at the root side of the central retaining screw of the internally connected implant prosthesis is a geometrically changed interface. The lever effect can lead to local stress concentration in this area, and the threads themselves also reduce the thickness of the implant wall. Once the screw loosens, the lever force of the abutment makes this area prone to fractures.




– Implant Position and Prosthesis Design
Studies have found that implants in the premolar area have the highest fracture proportion among all areas. The reason is that most full-arch fixed prostheses mainly rely on the implants in the premolar area and the anterior tooth area for support. The cantilever of the prosthesis is under long-term stress, thus increasing the risk of implant fractures. When the cantilever of the crown prosthesis supported by a single implant exceeds twice the diameter of the implant, the probability of mechanical complications of the implant will significantly increase. For fixed dentures supported by maxillary implants, the cantilever should be ≤ 10 mm, and for those supported by mandibular implants, the cantilever should be ≤ 15 mm.
When a single tooth is restored with an implant, poor crown morphology design, unfavorable crown-to-root ratio, and crown height space may all cause mechanical complications of the implant.
Clinically, it is considered that the optimal ratio of the tooth outside the alveolar bone to the tooth root inside the bone is 1:2. Increasing the crown length and non-axial occlusal stress will lead to excessive loading of the implant.
4.Surgical Treatments for Fractured Implants
– Implant Removal + Simultaneous Implant Placement
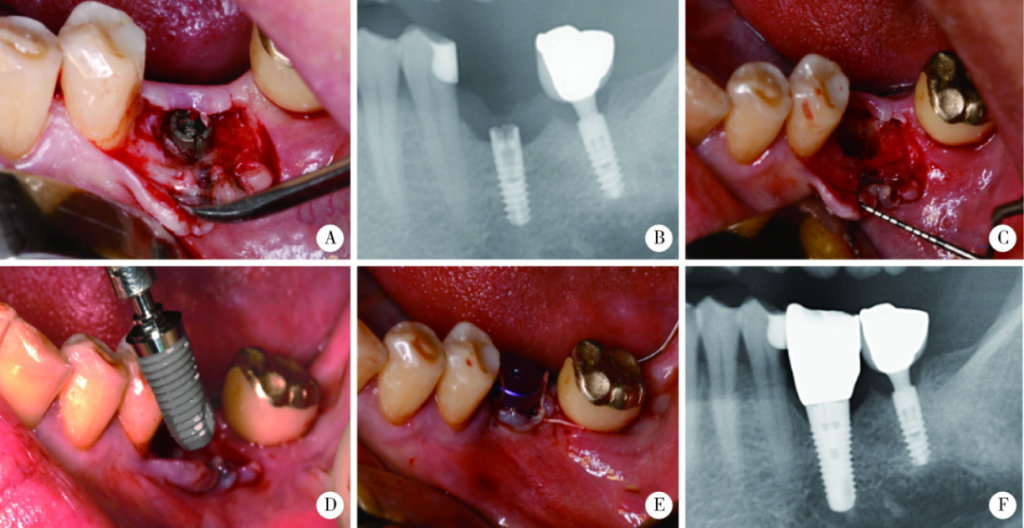
Use a fine fissure bur to remove the fractured implant to avoid bone loss around the implant (C). At the same time, insert a new implant with a larger diameter (Thommen SPI contact 6.0 mm x 11 mm) (D, E). The periapical X-ray evaluation 3 years later shows that the treatment result is stable (F).
– Implant Removal + Guided Bone Regeneration + Delayed Implant Placement
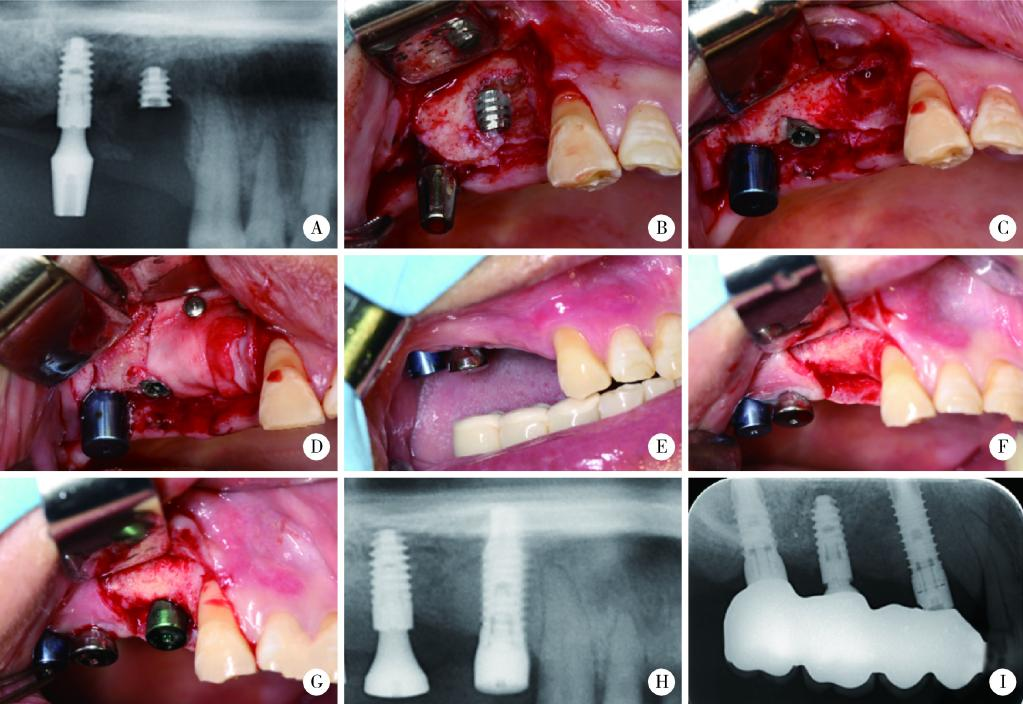
Use a fine fissure bur to remove the fractured implant (C). At the same time, perform guided bone regeneration (D). Six months later, the soft tissue heals (E) and the bone is repaired (F). Insert a new implant (Thommen SPI contact 4.3 mm x 12.5 mm) (G, H). The periapical X-ray film 3 years later shows the treatment effect (I).
– Implant Removal + Ectopic Implantation
For cases where it is not necessary to place the implant in situ, after removing the fractured implant, a new implant can be placed at other sites with better bone mass. The site after implant removal can heal naturally or undergo alveolar ridge preservation.
– Implant Shaping and Embedding
Incise and flap, remove the fractured end of the implant, use a round bur to trim the fracture surface of the implant to a smooth state, at least 3 mm below the crest of the alveolar bone, cover it with a collagen membrane and platelet-rich plasma, and suture the gingival flap with tension reduction.
– Fixed Partial Denture or Removable Partial Denture Restoration
After the implant is removed or the fractured end is embedded, fixed partial dentures or removable partial dentures can be designed and restored 3 months after healing.
5.Treatment Strategies for Fractured Central Screws
– Overview
The incidence of central screw fractures is only 0.6%. Screw fractures mostly occur in the molar area and the maxillary anterior tooth area, with the first mandibular molar being the most common. Before fracture, excessive stress is exerted, resulting in screw damage, especially at the screw head and the first thread. Therefore, the screw fracture line is mostly located on the screw body. If the implant has no retention value, it can be directly extracted. In cases where the implant needs to be retained, attempts can be made to remove the remaining parts of the fractured central screw.
– Treatment Plans
(1) Judging the Difficulty Level
The success rate of removing large-diameter screws is significantly higher than that of small-diameter screws.
It is easier to handle when the fracture line is located above the implant than when it is inside the implant.
If the fractured screw is broken due to excessive torque, it is more difficult to remove this screw. If the screw has been loose for a long time before fracture, it indicates that the fractured screw has a high probability of being loose and is relatively easy to remove.
(2) Improving the Visibility of the Surgical Area
The fractured screw can be observed, judged, and operated through direct vision, imaging examinations, magnifying glasses, microscopes, etc. Especially when the position of the fracture line is deep or the operator lacks experience, using a dental magnifying glass or microscope with a light source will greatly increase the success rate of removal.
If the prosthesis has been missing for a long time, the screw may have been covered by the soft tissue around the implant. If there is sufficient keratinized gingiva, circular excision or laser can be selected for trimming. If the keratinized gingiva is insufficient, it is more appropriate to incise and flap the soft tissue and fix the tissue flap with sutures.
– Low Difficulty Level
① If the fracture line is located above the implant, you can try to clamp the fractured end of the screw with tweezers or hemostatic forceps and unscrew it counterclockwise.
② If the fracture line is located inside the implant, you can first use a probe to check whether the screw is loose.
If it is loose, you can use a modified cotton swab to unscrew it counterclockwise, or you can also use some rigid tools. If the main body of the screw has been completely removed and only some threads remain, you can also try to use root canal files for operation.
When the screw is not very loose, ultrasonic vibration can also be used as an auxiliary method. When the fracture surface is inclined, place the tip of the ultrasonic device on the inclined surface and vibrate counterclockwise around the fracture surface to unscrew it from the screw channel. When the fracture surface is relatively flat, some studies have proposed that a 1-mm-deep hole can be prepared at a non-central position on the fracture surface with a round bur or an ultra-fine bur, place the tip of the ultrasonic device in the hole, and apply a reverse rotation force to unscrew the remaining fractured screw. There are also studies showing that while using ultrasonic vibration, a probe can be placed at a diagonal position and inserted into the gap between the screw and the implant to help loosen the screw.
In addition, there are also a few case reports that the fractured screw can be left untreated and only a shorter screw can be used for final restoration. In vitro studies have shown that when the length of the central screw is greater than 1.4 mm or the number of threads is more than 3.5, there is no significant relationship between its length and screw loosening or fracture. However, the current clinical case reports only have a 1-year follow-up, and longer follow-up results are needed to support the effect.
– Medium Difficulty Level
If the screw fragments cannot be removed by the methods for low difficulty level, other measures need to be considered. Mainly, reverse rotation tools are used for operation. The thread design direction of the reverse rotation tool is opposite to that of ordinary drill bits. The principle is that while the drill bit penetrates the screw fracture surface, it gives the screw a counterclockwise rotation force to unscrew it.
The tip of the reverse rotation grasping tool is generally “claw-shaped”. During the operation, the tip exerts pressure on the fracture surface in the hope of penetrating it. After engagement, the screw can be removed with a relatively small reverse rotation force. This method is more suitable for screws with a long history of loosening before fracture.
When the reverse rotation grasping tool cannot engage with the fracture surface, a small hole about 1 mm deep or a groove in the shape of a Chinese character “一” can be prepared in the center of the fracture surface with a round bur or a twist drill, and then the screw can be unscrewed with a modified reverse rotation screwdriver or bur.
When drilling holes and reverse rotation still cannot unscrew the screw, a third method can be chosen: directly grind the screw completely and use an internal thread forming tool to clean the remaining threads.
After removing the screw, it is usually necessary to judge the following two points:
(1) Whether the screw fragments are completely removed.
(2) Whether the internal thread structure of the implant is damaged.
Judgment methods:
(1) Microscopic observation
(2) Periapical film
(3) Screw in the healing abutment, and roughly judge whether the abutment is completely seated by checking whether it can be tightened and supplemented by taking X-rays.
(4) Use impression materials to make a negative mold of the internal thread structure of the implant and compare it with a normal implant for judgment.
– High Difficulty Level
If the internal thread of the implant is damaged, it is generally recommended to extract the implant and place a new one. If the patient is still unwilling to sacrifice the implant, there are three treatment methods:
Use the remaining threads for final restoration. Only use the remaining thread structure to make a short screw fixed prosthesis, and at the same time use two layers of washers to increase the pre-tightening force. There are case reports suggesting that if there are more than two internal thread structures in the implant, this technique can be used. However, this technique greatly reduces the number of retaining threads, and the long-term effectiveness of the washers and short screws is still unclear.
Re-make an internal thread with a larger diameter inside the implant. This operation requires professional internal thread forming tools for implants.
Grind off the internal thread to make a post channel. This method can be considered if the difference between the post length and the restoration space is small. This restoration method relies more on adhesive retention. Therefore, there are also literatures using inverted cone drills to prepare undercuts on the post to increase the retention force.
The latter two methods modify the implant, reducing the thickness of the implant arm and weakening the strength of the implant, so they should be used with caution.
References
[1] Chen Si, Chen Xinglin, Ma Wenjie, et al. Clinical Analysis of 10 Cases of Implant Fractures [J]. Stomatology, 2024, 44(01): 50-55. DOI: 10.13591/j.cnki.kqyx.2024.01.011.
[2] Li Yi, Wei Huajie, Qiu Lixin. Clinical Classification and Clinical Treatment Schemes for Implant Fractures [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 126-133.
[3] Lang NP, Pjetursson BE, Tan K, et al. A Systematic Review of the Survival and Complication Rates of Fixed Partial Dentures (FPDs) after an Observation Period of at Least 5 Years [J]. Clin Oral Implants Res, 2004, 15(6): 643-653.
[4] Stoichkov B, Kirov D. Analysis of the Causes of Dental Implant Fracture: A Retrospective Clinical Study [J]. Quintessence Int, 2018, 49(4): 279-286.
[5] Howe MS, Keys W, Richards D. Long-term (10-year) Dental Implant Survival: A Systematic Review and Sensitivity Meta-analysis [J]. J Dent, 2019, 84: 9-21.
[6] Zhu Yuqian, Zhou Yi. Treatment Strategies for Fractured Central Screws of Implants [J]. Chinese Journal of Practical Stomatology, 2024, 17(05): 537-541. DOI: 10.19538/j.kq.2024.05.006.




Leave a Reply