
All-ceramic materials possess superior aesthetic properties, mechanical properties, and biocompatibility, making them the most commonly used dental aesthetic restoration materials in clinical practice, especially in veneer restorations. Over the years, zirconia-based all-ceramic materials have undergone research, improvement, and development, with four generations of zirconia now applied in various oral restoration treatments. However, there remains some controversy regarding the use and selection of zirconia materials for all-ceramic veneers. This article aims to address the concerns and topics of interest to broad clinical dentists.
Author: Wan Qianbing
West China Hospital of Stomatology, Sichuan University
Can zirconia material be used to fabricate all-ceramic veneers?
Based on the advancements in zirconia materials and clinical case reports, the author’s current perspective is that 4Y zirconia (high-translucency zirconia) and 5Y zirconia (ultra-translucent zirconia) can be used for the fabrication of all-ceramic veneers, while 3Y zirconia (high-strength zirconia) is not suitable for making zirconia all-ceramic veneers. The zirconia materials currently used in clinical practice include(Table 1):
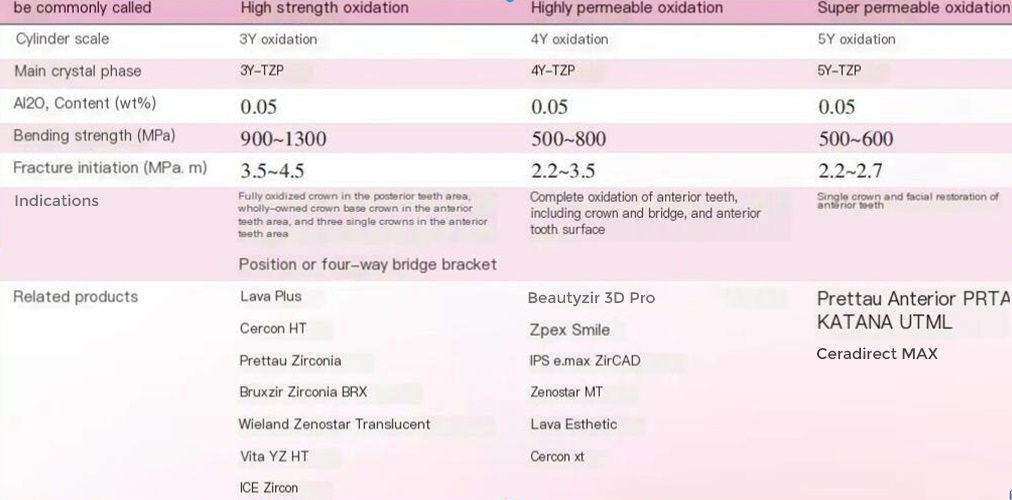
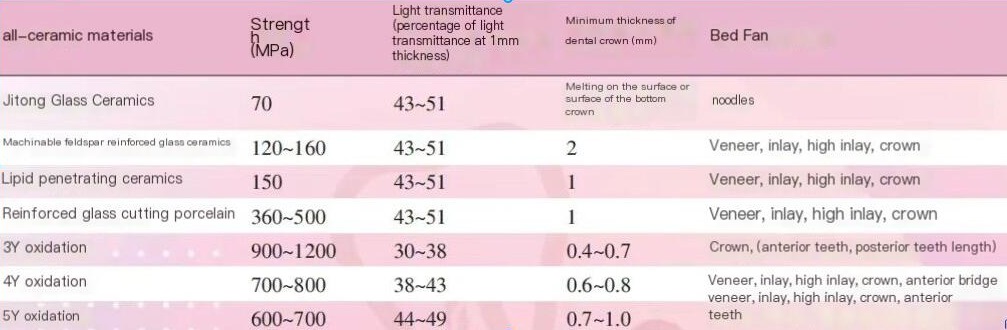
3Y Zirconia – Partially stabilized zirconia containing 3 mol% yttria (Y2O3) stabilizer, characterized by a phase transformation toughening mechanism, high strength (900MPa~1200MPa), and high toughness. However, due to the presence of different crystal phases, light refraction occurs at the interfaces between different crystal phase particles, resulting in generally poor light transmission.
4Y Zirconia – Partially stabilized zirconia containing 4 mol% Y2O3 stabilizer, which has improved translucency compared to 3Y zirconia materials, referred to as high-translucency zirconia (HT), but with slightly reduced strength (700MPa~800MPa).
5Y Zirconia – Partially stabilized zirconia containing 5 mol% Y2O3 stabilizer, with a higher proportion of cubic crystal phases. The fully stabilized cubic zirconia, due to identical crystal particle sizes, does not cause light refraction at the particle interfaces, thus having better translucency, referred to as super-translucent (ST) or ultra-translucent (UT) zirconia. However, due to the lack of a phase transformation toughening mechanism, the strength is lower (600MPa~700MPa), primarily used for restorations in the esthetic zone of anterior teeth.
From a translucency perspective, 4Y and 5Y zirconia materials can be used to fabricate all-ceramic veneers. Research shows that at a porcelain layer thickness of 0.5mm, the translucency of e-max CAD low-translucency zirconia (LT) is only about 20% higher than that of Katana UT ultra-translucent zirconia porcelain; at a porcelain layer thickness of 1.0mm, the translucency of e-max CAD LT zirconia is only about 15%~20% higher than that of Katana UT, Prettau Anterior, and Katana ST, indicating that the translucency of ultra-translucent zirconia materials is close to that of conventional glass-ceramic materials commonly used in veneer restorations, and can be used to fabricate anterior all-ceramic veneers.The basic properties of commonly used all-ceramic materials are shown in Table 2.
Can zirconia all-ceramic veneers be securely bonded?
The greatest challenge faced by zirconia veneers is the reliability of zirconia bonding. However, if the APC bonding method for zirconia bonding is strictly followed, including air-particle abrasion, pretreatment (zirconia Primer), and resin bonding (adhesive Composite resin), good bonding results can also be achieved. Especially when combined with a pretreatment agent containing MDP, it often basically meets the bonding requirements for veneers.
Although zirconia can be used for veneer fabrication, the bonding of zirconia all-ceramic has not yet reached the bonding effect of glass-ceramics.
Various technologies have been tried for the treatment of zirconia tissue surfaces to improve the bonding effect of zirconia restorations, such as alumina particle blasting technology, silicon film methods (including chemical friction method, sol-gel method, etc.), laser etching, and low-temperature plasma spraying technology.
However, these technologies have not been widely used in clinical practice due to poor effects and inconvenient operations. To address the bonding concerns of zirconia all-ceramic veneers, some domestic and international manufacturers have recently introduced zirconia all-ceramic veneer products that include the use of glass fusing technology to treat zirconia tissue surfaces (for example, the Bai Aomei treatment agent from Aidite and the zirconia adhesive from Beishimei are both low-melting point glass-ceramic materials, which are brushed or sprayed onto the tissue surface after the zirconia veneer is completed, and then sintered according to the glass-ceramic sintering procedure to fuse with the zirconia), achieving bonding effects similar to conventional glass-ceramic veneers. The principle is that through a simple glazing spraying technique, a layer of glass-ceramic with a lower melting temperature can be fused onto the tissue surface of zirconia, and this layer of glass-ceramic can be firmly combined with zirconia through a single low-temperature sintering. After surface modification of zirconia with glass fusing, its surface structure and composition are basically consistent with those of glass-ceramic materials, so the surface of zirconia treated with glass fusing can be etched with hydrofluoric acid for surface roughening, thereby producing reliable mechanical interlocking force and reliable chemical bonding force, which is the same as the bonding treatment steps for conventional glass-ceramic veneers.
Clinical implication: Mastering zirconia bonding technology is of great significance.
What conditions can zirconia all-ceramic veneers be used for?
Since the bonding of zirconia all-ceramic currently still has some uncertainties, why choose zirconia material for porcelain veneers? For strength or aesthetics?
The author believes that it should be more for its strength! Even with 5Y zirconia strength of about 600MPa, it is still about 50% higher than the strength of glass-ceramic materials, which is about 400MPa, especially since zirconia can be made into full-zirconia veneers without the need for veneer porcelain, generally not prone to chipping. Conversely, conventional porcelain veneers often have lower strength or have veneer porcelain covering their surface, making them more prone to chipping.
Secondly, it can mask the color of the underlying tooth. Juntavee et al.’s studies have shown that zirconia material has better color shading ability than glass ceramics, if you want to cover the color of tetracycline teeth, zirconia has a minimum thickness of 0.6mm, while zirconia reinforced lithium silicate ceramics has a minimum thickness of 1.2mm~1.6mm. so for tetracycline teeth that are obviously stained, zirconium oxide is a better choice for covering up discolored teeth and stained teeth.
In addition, zirconia all-ceramic veneers have the advantages of low production cost, easy CAD/CAM production, and lower technical sensitivity.
The indications for zirconia veneers recommended by the current authors are as follows:
(1) large interdental space;
(2) tightly occluded affected teeth;
(3) Anti-tooth;
(4)Darker colored affected teeth, such as deeply stained tetracycline teeth, need to be properly covered.
Contraindications are as follows:
(1) teeth with enamel underdevelopment;
(2) teeth that need to restore good translucency.
Clinical tip: Select appropriate cases when using zirconia all-ceramic veneers.
What are the clinical techniques for using zirconia veneers?
Currently, there are only a few clinical literature reports on the clinical application of zirconia veneers, showing good short-term clinical effects. However, to maintain long-term clinical effects, the author suggests paying attention to the following techniques in clinical practice:
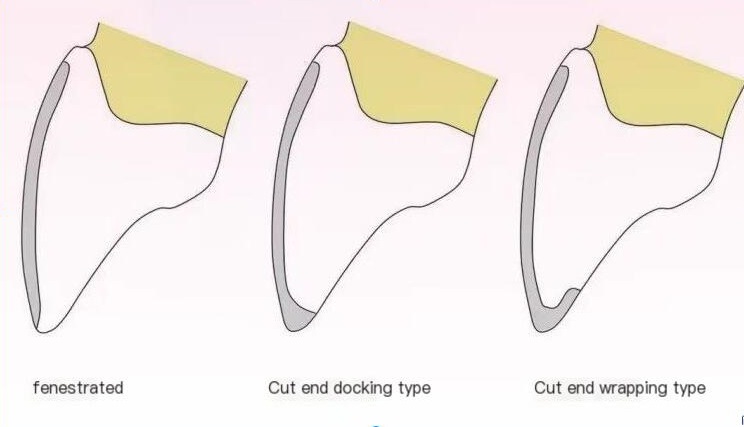
① It is recommended to choose window-type tooth preparation (Figure). Kusaba et al. conducted a study on the tooth preparation form for high-translucency zirconia veneers from the perspective of fit, and the results showed that the window-type incisal edge fit and tissue fit were better, possibly due to model scanning accuracy, cutting equipment limitations, and zirconia shrinkage after cutting and sintering. Another advantage of window-type tooth preparation is to avoid direct exposure to large occlusal forces.
② In terms of occlusal contact: It is recommended to have light occlusion or no contact.
③ Case selection: It is best not to restore teeth with too high translucency.
Prospect
With the advancement of zirconia all-ceramic materials, the translucency of the materials is further improved while maintaining appropriate high strength. If future researchers can solve the bonding problem of zirconia, perhaps the clinical application of zirconia all-ceramic veneers will become more and more widespread.
References
1. 万乾炳.口腔氧化锆修复材料分代之我见[J].国际口腔医学杂志,2021,48(02): 125-128.2. Harada K, Raigrodski AJ, Chung KH, Flinn BD, Dogan S, Mancl LA. A comparative evaluation of the translucency of zirconias and lithium disilicate for monolithic restorations. J Prosthet Dent. 2016 Aug;116(2):257-263.3. Matsuzaki F, Sekine H, Honma S, Takanashi T, Furuya K, Yajima Y, Yoshinari M. Translucency and flexural strength of monolithic translucent zirconia and porcelain-layered zirconia. Dent Mater J. 2015;34(6):910-917.4. Giordano Ii R. Ceramics overview. Br Dent J. 2022 May;232(9):658-663.5. Juntavee N, Juntavee A, Phetpanompond S. Masking ability of different ceramics upon various underlying structures. J EsthetRestor Dent. 2022 Mar;34(2):430-439.6. Kusaba K, Komine F, Honda J, Kubochi K, Matsumura H. Effect of preparation design on marginal and internal adaptation of translucent zirconia laminate veneers. Eur J Oral Sci. 2018 Dec;126(6):507-511.7. Souza R, Barbosa F, Araújo G, Miyashita E, Bottino MA, Melo R, Zhang Y. Ultrathin Monolithic Zirconia Veneers: Reality or Future? Report of a Clinical Case and One-year Follow-up. Oper Dent. 2018 Jan/Feb;43(1):3-11.




Leave a Reply