
Artificial intelligence (AI) is rapidly developing and has been widely applied in various fields.
The application of AI in the field of prosthodontics is mainly concentrated in the following three areas:
1. Image Recognition and Processing
1.1 X-ray and Panoramic Film Recognition
1. Automatic Tooth Position Recognition and Age Estimation

2. Oral Disease Recognition:
– Deep learning models can identify oral diseases such as caries, periapical diseases, tooth defects, retained roots, supernumerary teeth, etc., assisting in rapid diagnosis.

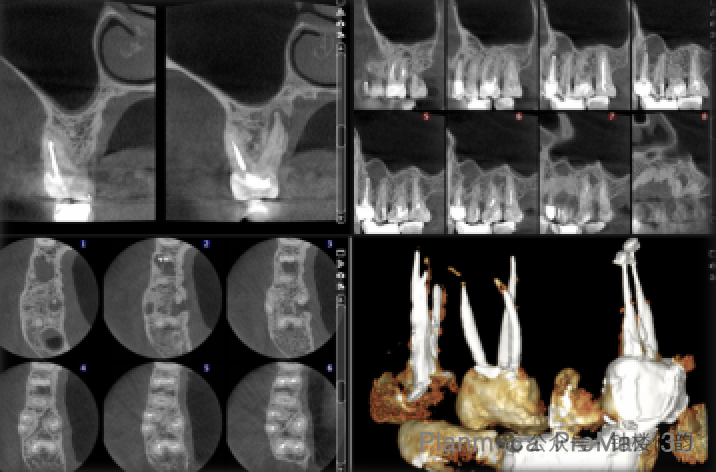
1.2 Automatic Segmentation of CBCT
CBCT imaging is the only way to provide comprehensive 3D volumetric information about the teeth and alveolar bone. Segmenting individual teeth and gingival bone structures from CBCT images to reconstruct accurate 3D models is crucial in digital dentistry. Fully automatic segmentation of teeth and alveolar bones is complex, comprising at least three main steps: region of interest (ROI) localization, tooth segmentation, and alveolar bone segmentation. Previous methods often focused on just one step, such as segmenting teeth or alveolar bones within predefined ROI regions. Moreover, they struggled with complex clinical cases like missing teeth, misalignment, and metal artifacts. Additionally, they were typically implemented and tested on very small datasets (10-30 CBCT scans), limiting their generalizability and applicability to CBCT images obtained through different imaging protocols and patient populations. The team of Dinggang Shen from the School of Biomedical Engineering, ShanghaiTech University, developed a fully automatic deep learning-based system for tooth and alveolar bone segmentation to address these clinical application limitations.

The system includes multi-level morphology-guided tooth segmentation networks and filter-enhanced alveolar bone cascade segmentation networks. The system’s segmentation evaluation metrics on external datasets showed Dice coefficients of 92.54% for teeth and 93.8% for alveolar bones, with sensitivities of 92.1% (teeth) and 93.5% (bones), and ASD errors of 0.21 mm (teeth) and 0.40 mm (bones).
In clinical practice, patients seeking dental treatment usually suffer from various dental problems, such as missing teeth, displacement, and intraoral metal implants. This system can also be applied to patients with missing and misaligned teeth, although it is slightly less effective in handling metal artifacts.
In addition to hard tissue segmentation, AI has also demonstrated its superiority in soft tissue segmentation. Accurately delineating the mandibular nerve canal range on CBCT images is crucial for preventing nerve damage during impacted tooth extraction, implant surgery, and orthognathic surgery. Traditional CBCT methods for tracking the mandibular nerve canal require manual marking along the nerve canal path to generate a fixed-diameter canal. This method relies on manual marking, which lacks accuracy and is extremely time-consuming, failing to meet the growing clinical demand.
Deep learning-based AI systems can achieve precise segmentation of the mandibular nerve canal in different models, including steps such as ROI extraction, overall segmentation of the mandibular nerve canal, and final local segmentation to refine the results. Performance on internal and external datasets has demonstrated its robustness and strong generalizability. The system also shows good segmentation results for complex cases, such as the compression of the nerve canal by the roots of the lower third molars.


2. Assisted Design of Restorations
2.1 Assisted Design of Full-Crown Restorations
Professor Jiefei Shen’s team from West China School of Stomatology developed an AI system using deep learning technology for the individualized automatic completion of tooth defect morphology.

Other applications include the design of crown margins, overall morphology, and occlusal surface morphology.



2.2 Automatic Design System for Removable Partial Dentures (RPD)
Traditional RPD design relies on experienced technicians or dentists to complete manually, which is time-consuming and prone to errors. AI technology, especially deep learning-based image analysis and CAD (Computer-Aided Design) technology, can quickly generate patient-specific RPD designs, reducing human error.

2.3 Predicting Bonding Strength and Longevity of Restorations

2.4 Development of New Dental Materials
Over the past 40 years, CAD/CAM materials used in dentistry have significantly developed. Researchers have been combining AI (especially machine learning) with traditional experimental methods to discover the relationships between the properties of restorative materials and various physical factors. Compared to traditional experimental methods, machine learning is a faster method as it can quickly evaluate and analyze collected data, extract relevant features, save time, accelerate the design process of new materials, and improve material quality.

3. Intelligent Dialogue Models and Smart Devices
3.1 Intelligent Oral Dialogue Models
Natural Language Processing (NLP) technology can analyze patient-submitted symptoms and provide suggestions, but its application in dentistry still needs optimization. As NLP advances, intelligent dialogue models will play a larger role in oral care and management.

3.2 Intelligent Oral Devices


With the continuous development of AI technology, the degree of digitization and intelligence in the dental field will increasingly advance. Based on online patient-doctor platforms and intelligent consultation systems, from high-precision data collection and processing to fully automated virtual patient construction, comprehensive data analysis, disease diagnosis, intelligent treatment plan design, treatment effect prediction, and high-precision treatment implementation as planned, to automatic detection of the treatment process and follow-up. Prosthodontics will further develop with the assistance of AI.
Main References:
[1]Shen S, Yuan X, Wang J, Fan L, Zhao J, Tao J. Evaluation of a machine learning algorithms for predicting the dental age of adolescent based on different preprocessing methods. Front Public Health. 2022 Dec 1;10:1068253.[2]Kim C, Jeong H, Park W, Kim D. Tooth-Related Disease Detection System Based on Panoramic Images and Optimization Through Automation: Development Study. JMIR Med Inform. 2022 Oct 31;10(10):e38640.
[3]Cui Z, Fang Y, Mei L, Zhang B, Yu B, Liu J, Jiang C, Sun Y, Ma L, Huang J, Liu Y, Zhao Y, Lian C, Ding Z, Zhu M, Shen D. A fully automatic AI system for tooth and alveolar bone segmentation from cone-beam CT images. Nat Commun. 2022 Apr 19;13(1):2096.
[4]Ni FD, Xu ZN, Liu MQ, Zhang MJ, Li S, Bai HL, Ding P, Fu KY. Towards clinically applicable automated mandibular canal segmentation on CBCT. J Dent. 2024 May;144:104931.
[5]Chen D, Yu MQ, Li QJ, He X, Liu F, Shen JF. Precise tooth design using deep learning-based templates. J Dent. 2024 May;144:104971. doi: 10.1016/j.jdent.2024.104971.
[6]Choi J, Ahn J, Park JM. Deep learning-based automated detection of the dental crown finish line: An accuracy study. J Prosthet Dent. 2023 Dec 13:S0022-3913(23)00769-2. doi: 10.1016/j.prosdent.2023.11.018.
[7]Ding H, Cui Z, Maghami E, Chen Y, Matinlinna JP, Pow EHN, Fok ASL, Burrow MF, Wang W, Tsoi JKH. Morphology and mechanical performance of dental crown designed by 3D-DCGAN. Dent Mater. 2023 Mar;39(3):320-332.
[8]Fueki K, Inamochi Y, Wada J, Arai Y, Takaichi A, Murakami N, Ueno T, Wakabayashi N. A systematic review of digital removable partial dentures. Part I: Clinical evidence, digital impression, and maxillomandibular relationship record. J Prosthodont Res. 2022 Jan 11;66(1):40-52.
[9]Takaichi A, Fueki K, Murakami N, Ueno T, Inamochi Y, Wada J, Arai Y, Wakabayashi N. A systematic review of digital removable partial dentures. Part II: CAD/CAM framework, artificial teeth, and denture base. J Prosthodont Res. 2022 Jan 11;66(1):53-67.
[10]Yamaguchi S, Lee C, Karaer O, Ban S, Mine A, Imazato S. Predicting the Debonding of CAD/CAM Composite Resin Crowns with AI. J Dent Res. 2019 Oct;98(11):1234-1238.
[11]Li M, Dai L, Hu Y. Machine Learning for Harnessing Thermal Energy: From Materials Discovery to System Optimization. ACS Energy Lett. 2022 Oct 14;7(10):3204-3226.
[12]Kuroiwa T, Sarcon A, Ibara T, Yamada E, Yamamoto A, Tsukamoto K, Fujita K. The Potential of ChatGPT as a Self-Diagnostic Tool in Common Orthopedic Diseases: Exploratory Study. J Med Internet Res. 2023 Sep 15;25:e47621.
[13]Büttner M, Leser U, Schneider L, Schwendicke F. Natural Language Processing: Chances and Challenges in Dentistry. J Dent. 2024 Feb;141:104796.




Leave a Reply