
The majority of salivary calculi (80%) are found in the submandibular gland and duct. Another 10% occur in the parotid gland, with the remaining 10% in the sublingual and minor salivary glands. Bilateral or multiple-gland sialolithiasis is rare, occurring in less than 3% of cases. In patients with multiple stones, calculi can be found at different positions along the salivary duct and gland. Submandibular stones near the gland hilum often grow large before causing symptoms. Sialolithiasis is equally common on the right and left sides. Typically, sialoliths measure between 1 mm and 1 cm. Giant salivary gland stones (GSGS) are defined as those exceeding 1.5 cm and are rarely mentioned in medical literature. Stones over 3 cm are extremely rare, with only a few reported cases.
Case Report
In 2010, a 53-year-old white male was referred to the Oral and Maxillofacial Surgery Department at Damascus General Hospital. He presented with a large, firm mass on the left side of the floor of his mouth in the submandibular gland area, with a history of left submandibular swelling occurring during meals. His past medical history was unremarkable.
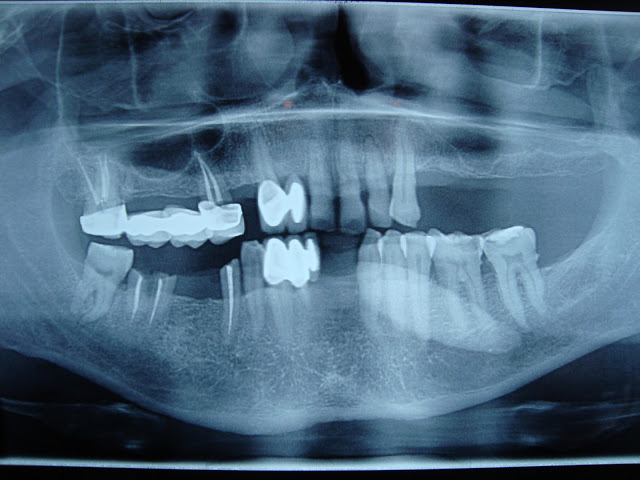
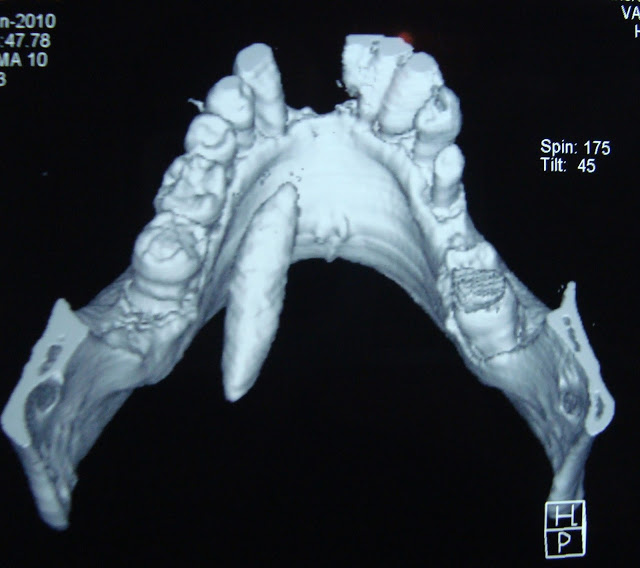
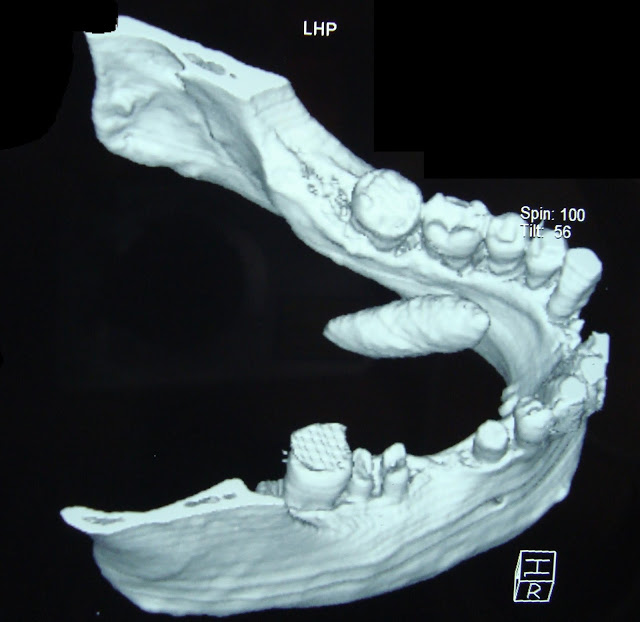
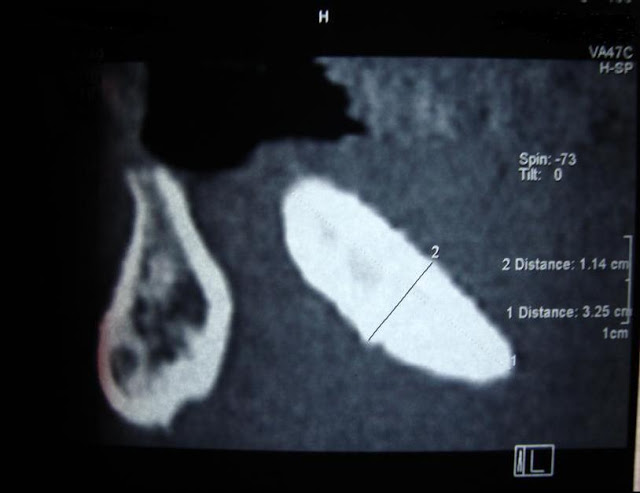
Examination revealed a mobile, firm, non-tender mass in the left submandibular salivary gland duct area, with swelling of the mouth floor. OPG showed a large calcified mass in that region. A CT scan revealed a 3.32*1.14 cm calculus obstructing the submandibular gland duct. Blood and serum biochemistry results were normal.

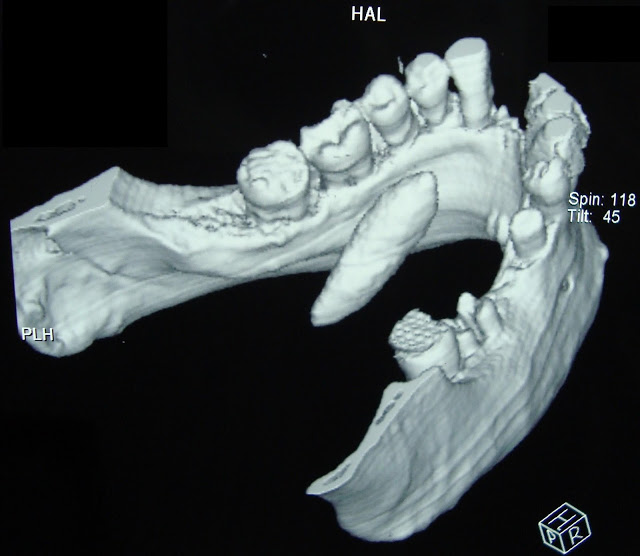

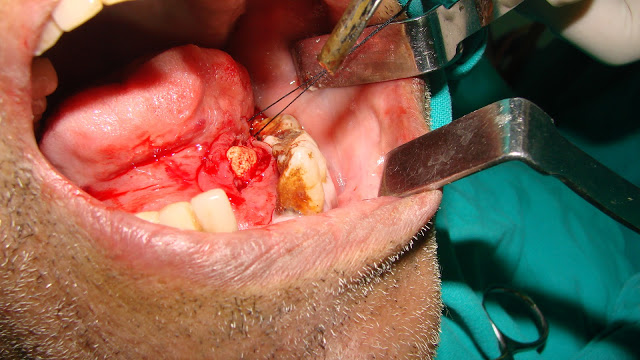
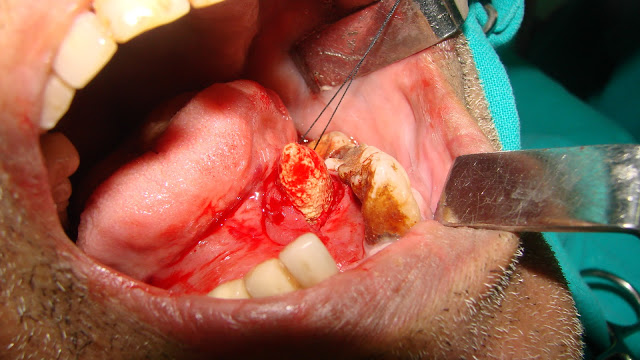
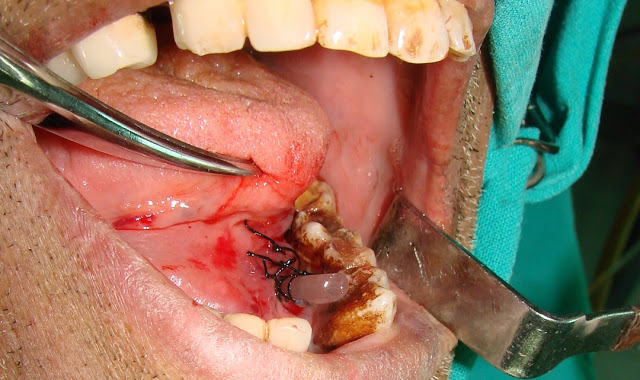
Under local anesthesia, the calculus was excised through an incision in the mouth floor directly over the palpable mass. The yellowish calculus was oval with a rough, irregular surface. A short polyethylene tube was inserted at the incision site, and the flap was sutured around the tube. The sutures and tube were removed after two weeks.


Discussion
Most salivary calculi (80%) are located in the submandibular gland and duct, with 10% in the parotid gland and 10% in the sublingual and minor salivary glands. Factors such as saliva flow against gravity, alkaline pH, and high mucin and calcium content may contribute to stone formation in the submandibular gland. The exact etiology and pathogenesis remain unclear, with a slight male predilection usually over the age of 40. Patients typically experience pain, discomfort, and swelling before or during meals, with recurrent submandibular swelling. Bimanual massage of the affected gland and duct should observe the flow and clarity of saliva. The calculus is often located in the excretory duct, causing characteristic pain. Submandibular gland calculi are radiopaque in 80-94.7% of cases. An occlusal radiograph can reveal the calculus in the anterior mouth floor. Ultrasonography is effective in detecting salivary stones larger than 2 mm as echodense spots, though small calculi detection may be challenging. CT is also highly diagnostic.
In cases where the submandibular gland is involved, a panoramic radiograph can be helpful. Small and radiolucent calculi may not be visible radiographically, making sialography a potential examination choice, though calculus displacement towards the gland may occur.
Large sialoliths in salivary glands or ducts, especially those over 3 cm, are rare. A review by Ledesma-Montes et al. found only 16 cases of stones 3.5 cm or larger. Sialoliths are usually ovoid or round, smooth or rough, and yellowish. They are composed of calcium phosphate with small amounts of hydroxyapatite, magnesium, potassium, and ammonia.
Surgical removal is common for submandibular stones, either intraorally or externally. If calculi are in the gland, extracorporeal or endoscopic laser lithotripsy can be performed multiple times. Post-removal or lithotripsy, scintigraphic exams show gland functional recovery. In non-functioning glands, surgical removal is necessary to avoid recurrent disease, and gland removal may be the first treatment choice in many units.
Future advancements hold promise for non-surgical, non-invasive techniques like shock wave lithotripsy, basket retrieval, and endoscopic laser lithotripsy. A review of over 4,691 patients by Iro et al. reported that stones less than 5 mm are usually retrieved with baskets or microforceps, while extracorporeal lithotripsy is mainly used for fixed parotid stones under 7 mm in diameter.
Conclusion
This case highlights the rarity of large calculus, which can be prevented by early diagnosis and proper treatment. Minimally invasive techniques should be considered for salivary gland stone removal upon diagnosis.
References
1- Seifert G, Mann W, Kastenbauer E 1992 Sialolithiasis. In :Naumann HH, Helms J, Herberhold C, Kastenbauer E (eds) Oto-Rhino-Laryngologie in Klinik und Praxis, Bd 2. Thieme, Stuttgart, pp 729-732
2- McKenna JP, Bostock DJ, McMenamin PG. Sialolithiasis. Am Fam Physician 1987 Nov;36: 119-25.
3- Bodner L. Giant salivary gland calculi: diagnostic imaging and surgical management. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002 Sep;94(3):320-3
4- Soares EC, Costa FW, Pessoa RM, Bezerra Giant salivary calculus of the submandibular gland. Otolaryngol Head Neck Surg. 2009 Jan;140(1):1289.
5- Ledesma-Montes C, Garcés-Ortíz M, Salcido-García J, Hernández-Flores F, Hernández-Guerrero H. Giant Sialolith, Case report and review of literature. J Oral Maxillofac Surg 2007; 65:128-30.
6- Peel RL, Gnepp DR 1985 Diseases of the Salivary Glands. In: Barnes L (ed) Surgical pathology of the head and neck, vol 1. Dekker, New York 533—645.
7- Lustmann J, Rege V, Mlelamed Y 1990 Sialolithiasis. A survey on 245 patients and a review of the literature. International Journal of Oral and MaxilloCcial Surgery 19:135—138.
8- Zakaria MA. Giant calculi of the submandibular salivary gland. Br J Oral Surg 1981 Sep;19: 230-2.
9- Marchal F, Kurt AM, Dulgerov P, Lehmann W. Retrograde theory in sialolithiasis formation. Arch Otolaryngol Head Neck Surg 2001 Jan;127: 66- 8.
10- Williams MF. Sialolithisis. Otolaryngol Clin North Am 1999 Oct;32: 819-34.
11- Van den Akker HP. Diagnostic imaging in salivary gland disease. Oral Surg Oral Med Oral Pathol 1988 Nov;66: 625-37.
12- Weissman JL. Imaging of the salivary glands. Semin Ultrasound CT MR 1995 Dec;16: 546-68.
13- Akin I, Esmer N. A submandibular sialolith of unusual size: A case report. J Otolaryngol 1991 Aor;20: 123-5.
14- Siddiqui SJ. Sialolithiasis: An unusually large submandibular salivary stone. Br Dent J 2002 Jul;193: 89-91.
15- Zenk J, Constantinidis J, Al-Kadah B, Iro H. Transoral removal of submandibular stones. Arch Otolaryngol Head Neck Surg. 2001 Apr;127: 432-6.
16- Marchal F, Dulguerov P. Sialolithiasis management, The state of the art. Arch Otolaryngol Head Neck Surg. 2003 Sep;129: 951-6.
17- Iro H, Benzel W, Zenk J et al 1993 Minimal-invasive Behandlung der Sialolithiasis mittels extrakorporaler StoBwellen. HNO 41:311—3 16.
18- Kater W, Rahn R, Meyer WW et al 1990 Ambulante extrakorporale StoBlwellenlithotripsie von Speichelsteinen als neues nichtinvasives Behandlungskonzept. Deutsche Zeitschrift für Mund-, Kiefer und Gesichtschirurgie 14:216—220.
11
19- Nahlieli 0, Neder A, Baruchin AM 1994 Salivary gland endoscopy: a new technique for diagnosis and treatment of sialolithiasis. Journal of Oral and Maxillofacial Surgery 52:1240—1242.
20- Ottaviani F, Capacio P, Campi M, Ottaviani A. Extracorporeal electromagnetic shock-wave lithotripsy for salivary gland stones. Laryngoscope 1996 Jun;106: 761-4.
21- Iro H, Zenk J, Escudier MP, Nahliell O, Capaccio P, Katz P, Brown J & McGurk M. Outcome of minimally invasive management of salivary calculi in 4,691 patients. The Laryngoscope 2009 Feb;119(2):263-8.
by Dr. Moutaz Al khen, Dr. Bader E. Abdeen




Leave a Reply