How can we achieve a strong bond between ceramic restorations and the tooth structure? This is one of the key factors for the success of all-ceramic restorations. This article will detail the mechanisms and methods of bonding technology.
All-ceramic crowns are ideal restorations due to their stable and natural color and excellent biocompatibility. Their clinical application is increasingly widespread. Currently, ceramic restorations used in clinical practice have good mechanical properties. Therefore, the bonding strength between ceramic restorations and tooth structure is crucial for the success of the restorations. Here, we summarize the current research on bonding systems.
Understanding the mechanism of bonding force formation is fundamental to mastering the correct bonding techniques. Let’s delve into the key and necessary conditions for achieving a bond:
1. Mechanism of Bonding Force Formation
Bonding force is the continuous force generated by the mutual attraction between the adhesive and the surface of the substrates. When an adhesive bonds two substrates together, a bonding interface is formed. In most cases, the bonding interface is a multiphase system with three homogeneous phases, including the adhesive and the two substrates, and the interfaces between them. Bonding force typically comprises four types: chemical bond force, intermolecular forces, electrostatic attraction, and mechanical interlocking.
Many scholars believe bonding force results from the mutual attraction between the adhesive and substrate molecules at the interface, encompassing physical adsorption and chemical adsorption. This adsorption theory, widely accepted today, explains that bonding force is produced by the combined action of intermolecular and atomic forces. The closer the distance between the adhesive molecules or atoms and the substrate, the greater the interaction force, leading to higher bonding strength. Only when the adhesive liquid adequately wets the substrate surface can the distance between them reach a range where effective valence bond forces are generated. This is the key and necessary condition for achieving bonding.
2. Adhesives
What are the commonly used adhesives in clinical practice?
2.1 Cement Adhesives
Cement adhesives mainly include zinc phosphate cement, zinc polycarboxylate cement, and glass ionomer cement. These adhesives primarily bond with the tooth structure and have no bonding capability to ceramic restorations.
2.1.1 Zinc Phosphate Cement
Zinc phosphate cement is a paste with certain fluidity before setting, allowing it to infiltrate the fine structures on the surfaces of the tooth and restoration, forming some mechanical interlocking. However, zinc phosphate cement releases free phosphoric acid during and after setting, which may irritate the pulp and gingiva. Due to its low bonding strength and strong irritation, its clinical application is limited. Research by Xin Hua Guo et al. found significant defects in the bonding layer of all-ceramic crowns bonded with zinc phosphate cement, with more defects appearing after chewing simulation tests, further limiting its clinical use.
2.1.2 Zinc Polycarboxylate Cement
Zinc polycarboxylate cement forms mechanical interlocking with the tooth and restoration. Additionally, -COOH groups that have not reacted can form hydrogen bonds with -OH groups on the tooth surface and chelate to some extent with Ca2+ in the tooth structure. The dissociated COO- groups can also generate ionic attraction with Ca2+ in the tooth. Therefore, its bonding strength is higher than that of zinc phosphate cement.
2.1.3 Glass Ionomer Cement
Due to its good bonding properties, biological safety, anti-caries effect, and resistance to dissolution, glass ionomer cement is widely used.
2.2 Composite Resin Adhesives
These adhesives have similar compositions and characteristics to traditional restorative resins, comprising organic matrixes (such as Bis-GMA, TEGDMA, and UDMA) and inorganic fillers. They can be classified into self-curing (chemical curing), light-curing, and dual-curing types based on curing methods. Compared to commonly used clinical adhesives, resin adhesives for all-ceramic restorations have good translucency, high bonding strength, resistance to dissolution in the oral environment, and good color matching. They can securely bond ceramic restorations to the tooth structure, ensuring long-term stable retention and effectively transmitting and dispersing applied stress to the tooth structure, playing a physiological role. Common resin adhesives for ceramic restorations include BIS-GMA and modified composite resins containing phosphoric acid monomers.
2.3 Hybrid Adhesives
These adhesives are composites of resin and glass ionomer, combining the advantages of both. Easy to use, they exhibit minimal volume shrinkage during setting, good sealing properties, reduced microleakage and secondary caries, stable color, durability, and good biocompatibility and strength. Research on hybrid adhesives has become a focal point in the study of adhesives.
3. Surface Treatment Techniques
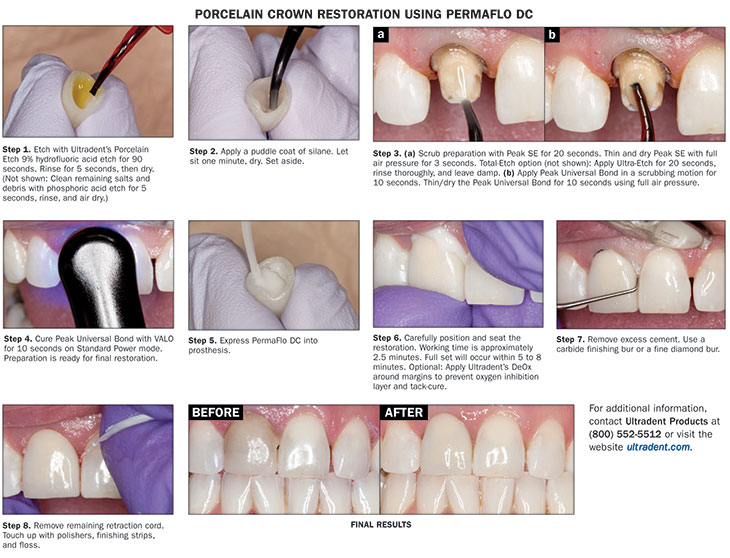
Composite resin adhesives mainly bond with ceramics and are widely used in clinical practice. The bonding strength between ceramic restorations and resin adhesives closely relates to various surface treatment methods. Different all-ceramic materials require different surface treatment methods to achieve optimal bonding. Bonding between ceramics and resins typically employs two mechanisms: micro-mechanical interlocking through HF etching or sandblasting the ceramic surface, and chemical bonding using silane coupling agents.
3.1 Etching Technique
Commonly, hydrofluoric acid is used to treat surfaces, achieving satisfactory bonding strength despite different concentrations and durations. Treating with 2.5%-10% hydrofluoric acid for 2-3 minutes yields good results. IPS Empress ceramics, rich in leucite, require 9% hydrofluoric acid etching for 60 seconds. Etching creates micro-grooves, cleaning and enlarging the bonding surface to obtain a rough surface structure, reducing surface tension. Kato et al. compared different etchants and sandblasting effects, finding that hydrofluoric acid and sulfuric acid hydrofluoric acid offer the highest and most durable bonding strength.
3.2 Sandblasting
Sandblasting increases the surface roughness of ceramics, enlarging the bonding area and forming micro-roughness that generates mechanical interlocking, thus enhancing bonding strength. Some scholars disfavor sandblasting feldspathic ceramics, as it may damage the surface bonding layer and reduce bonding strength. However, ceramics based on alumina (In-Ceram Alumina, GI-II infiltrated ceramics, etc.) are suitable for sandblasting due to their minor feldspathic content, high strength, minimal impact on surface structure, and reduced surface component loss. Clinically, 110μm Al2O3 sandblasting with 0.24MPa pressure is common. Madani et al. found that sandblasting In-Ceram ceramics with Al2O3 yielded higher bonding strength compared to HF etching.
3.3 Silane Coupling Agent Application
Silane coupling agents easily bond with glass ionomers primarily composed of SiO2 and Al2O3, forming stable siloxanes. The organic functional groups at the other end of the silane can co-polymerize or intertwine with resin molecules, tightly bonding ceramics to composite resin adhesives. Studies by Lacy et al. showed that sandblasting traditional silicate ceramics without coupling agents does not enhance retention. Sorensen et al. suggested that etching and silane treatment of ceramics significantly reduce microleakage, but silane treatment alone is insufficient. Some scholars recommend combining sandblasting (50μm Al2O3), HF etching, and silane treatment.

4. Surface Modification Treatment
SiO2 coatings enable chemical bonding between ceramics and resins through silane coupling agents. Two methods achieve this:
1. **Chemical Friction Method (e.g., Rocatec System):** After sandblasting with 110μm Al2O3, a second sandblasting with Rocatec-plus powder occurs. This powder, composed of irregularly shaped Al2O3 particles and regularly shaped SiO2 particles, bonds SiO2 to the treated surface through friction.
2. **Thermal Treatment Method (e.g., Silicoater System):** After 110μm Al2O3 sandblasting, the surface is coated with Cr2O3-containing SiO2 particles, bonding SiO2 to the surface through sintering. The PyrosilPen technology, an improvement of the Silicoater technology, is effective for treating alumina and zirconia ceramic surfaces and has proven effective on various dental alloys.
Though these methods differ, both aim to increase the SiO2 content on the surface of infiltrated ceramics, ensuring a stable bond between SiO2 and the ceramics.
Conclusion
All-ceramic restorations are made from materials like alumina, zirconia, and feldspathic ceramics. Due to their different surface properties, the same adhesive and surface treatment methods yield varying bonding strengths. Ideal adhesives for all-ceramic restorations should have low viscosity, excellent flowability, minimal thickness impact on restoration placement, high strength, and wear resistance. Surface treatment methods should be simpler and more effective.




Leave a Reply