Author:
Dr. Hajo Peters (Austria)
This case report details a year-long surgical and restorative treatment for a 24-year-old male patient. This patient had specific dental characteristics and underwent an implant restoration (CAMLOG®
SCREW-LINE) for a missing anterior tooth, followed by a one-year follow-up. As a professional musician, the patient had unique functional and aesthetic requirements. Treatment was carried out based on the Viennese esthetic protocol proposed by master dental technician Christian Koczy and dentists Dr. Otto Exenberger and Dr. Hajo Peters. This interdisciplinary collaboration among dental technicians, restorative dentists, and surgeons is evident in numerous detailed steps. The article describes the diagnosis and detailed clinical procedures: extraction of a maxillary anterior tooth with an apical cyst, cyst removal, temporary restoration, alveolar ridge reconstruction, implantation, soft tissue augmentation, contouring, and the final placement of a personalized all-ceramic restoration.
**Medical History and Clinical Examination**
A 22-year-old male patient underwent a routine examination in 2014, with a panoramic X-ray revealing a large radiolucent area in the maxillary anterior region. Despite being asymptomatic, a clinical examination of the soft and hard tissues revealed no significant abnormalities (Figure 1).

The patient, a professional saxophonist, reported occasional upper lip sensitivity, which he attributed to daily instrumental practice and overuse of the lip muscles. The dental history revealed that tooth #11 had undergone endodontic treatment five years earlier due to mechanical trauma leading to displacement. Initial splinting and subsequent pulp vitality tests indicated no re-innervation or re-vascularization, necessitating root canal therapy.
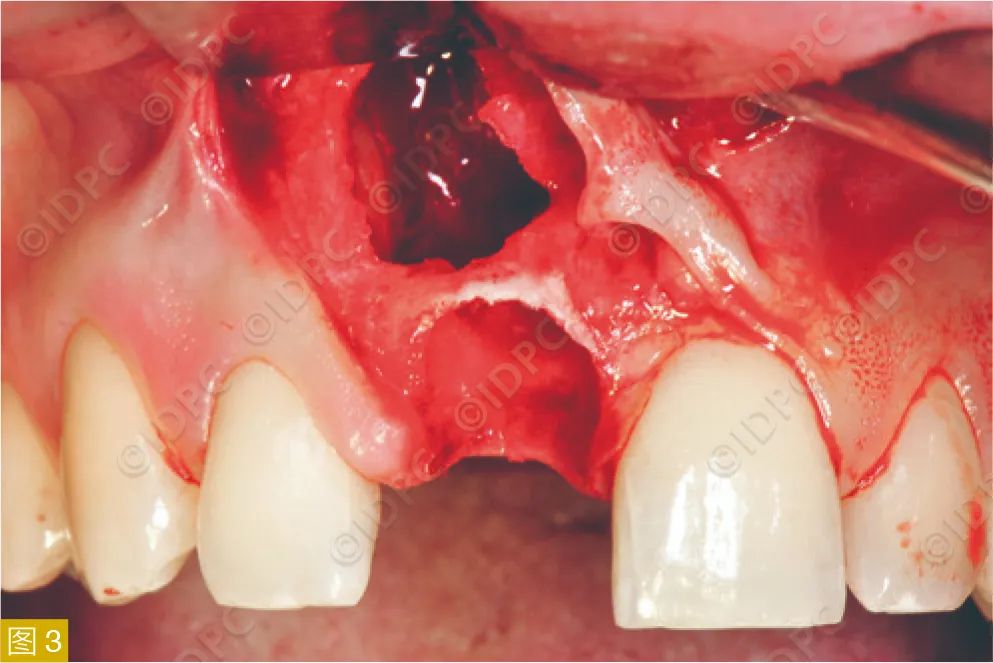
To better evaluate the suspected apical lesion, a three-dimensional imaging diagnosis was performed. The images revealed extensive bone loss: a 2×3×1 cm radiolucency associated with tooth #11, with bony erosion of the incisive foramen and a large labial defect visible in sagittal sections (Figure 2).
**Surgical Treatment**
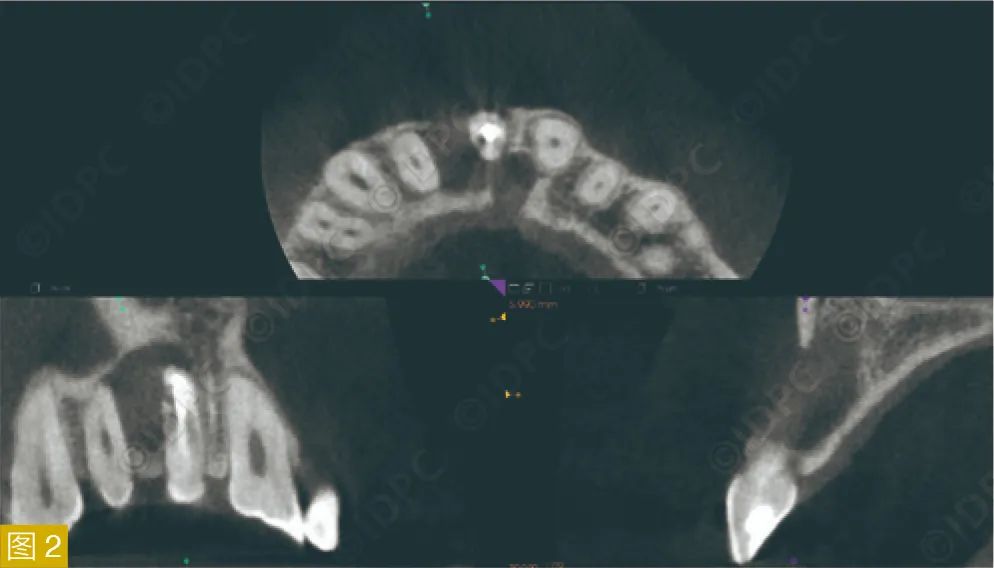
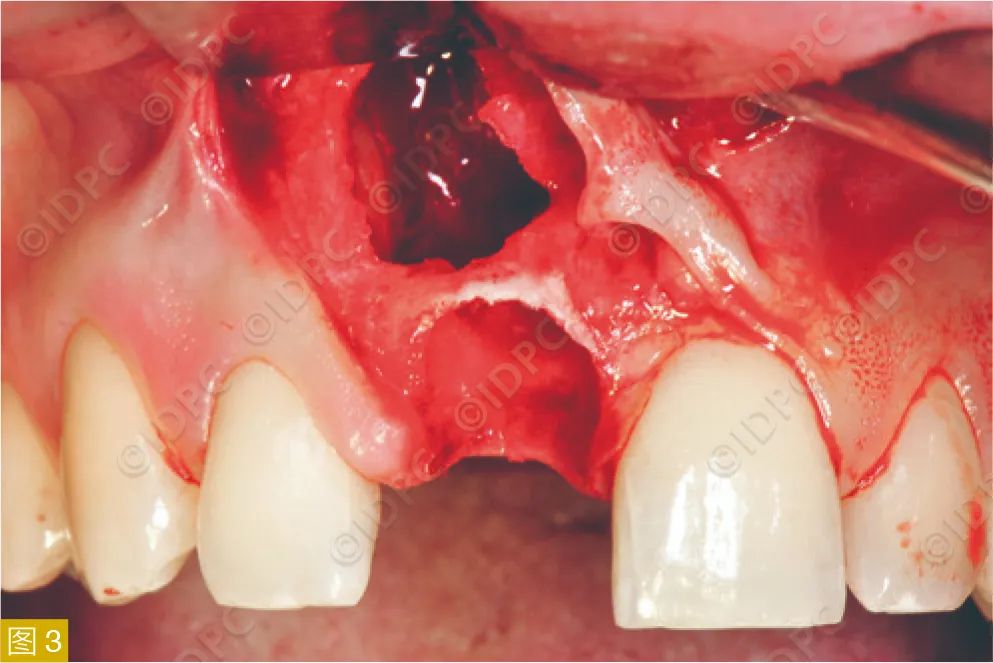
Subsequent surgery confirmed nearly complete labial bone loss (Figure 3). Using a piezosurgery device (mectron, Germany), the tooth was atraumatically extracted, preserving the coronal bone bridge. A pedicled mucoperiosteal flap facilitated pathology assessment and protected gingival papillae. The infected cyst was excised and histologically examined, confirming complete removal. A collagen plug (Parasorb, Resorba, Germany) was placed in the socket to stabilize the blood clot (Figure 5).


**Soft Tissue Healing and Temporary Restoration**
After soft tissue healing, the clinical examination revealed expected vertical and horizontal tissue loss. Despite well-healed and non-inflamed gums and mucosa, the aesthetic deficit was evident (Figure 6). Throughout the treatment, a vacuum-formed splint served as the patient’s temporary restoration (Figure 7).


**Bone Augmentation**
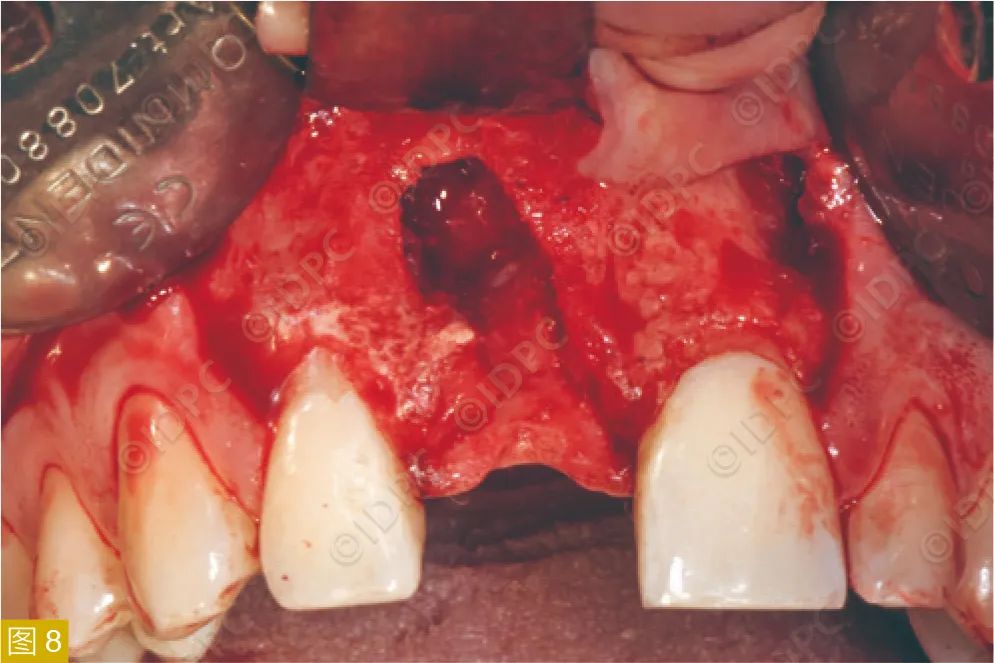
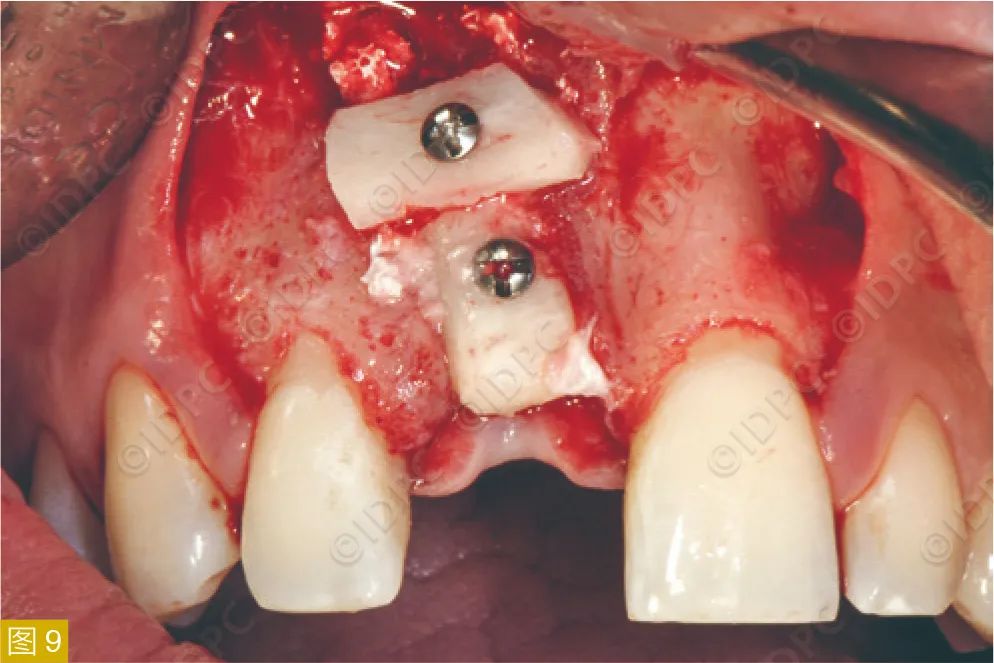
Four months later, the surgical site was reopened, revealing extensive bone loss, even in the previously preserved coronal bone bridge (Figure 8). The necessity for bone augmentation was explained to the patient before extraction, emphasizing its unpredictability in maxillary cancellous bone compared to mandibular cortical bone.
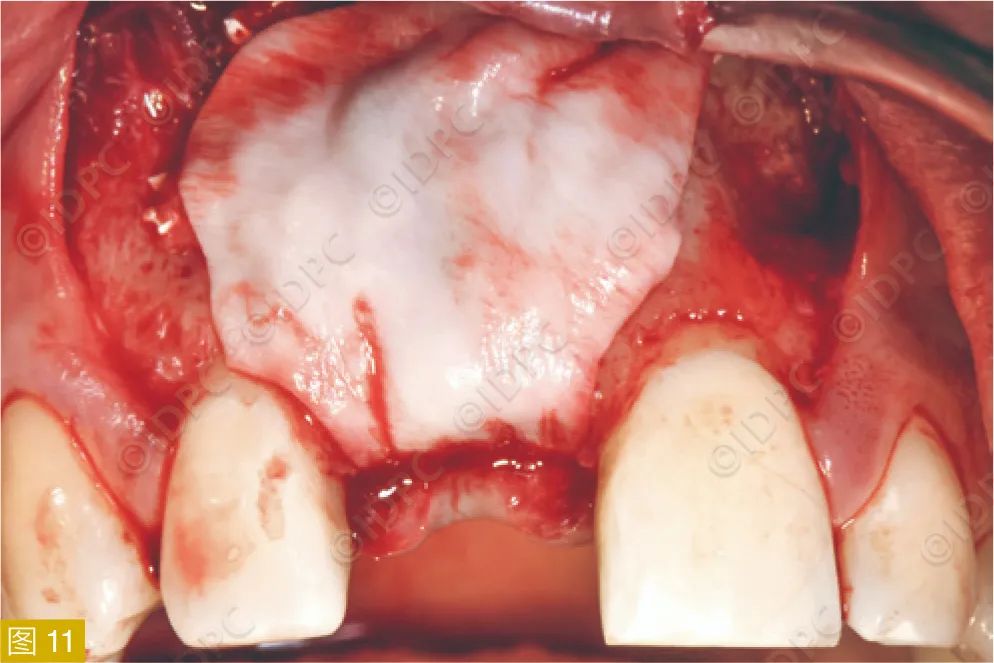
Two autogenous bone blocks were harvested from the right mandibular ramus under local anesthesia and used to augment the defect (Figure 9). The blocks were shaped using a trephine and fixed with bone screws (Ustomed, Germany) to ensure stability (Figure 10). The augmented area was then covered with a mixture of autogenous bone chips and xenogeneic bone substitute material (Bio-Oss®
, Geistlich) and a resorbable collagen membrane (Bio-Gide®, Geistlich) for guided bone regeneration (Figure 11).

**Implant Placement**
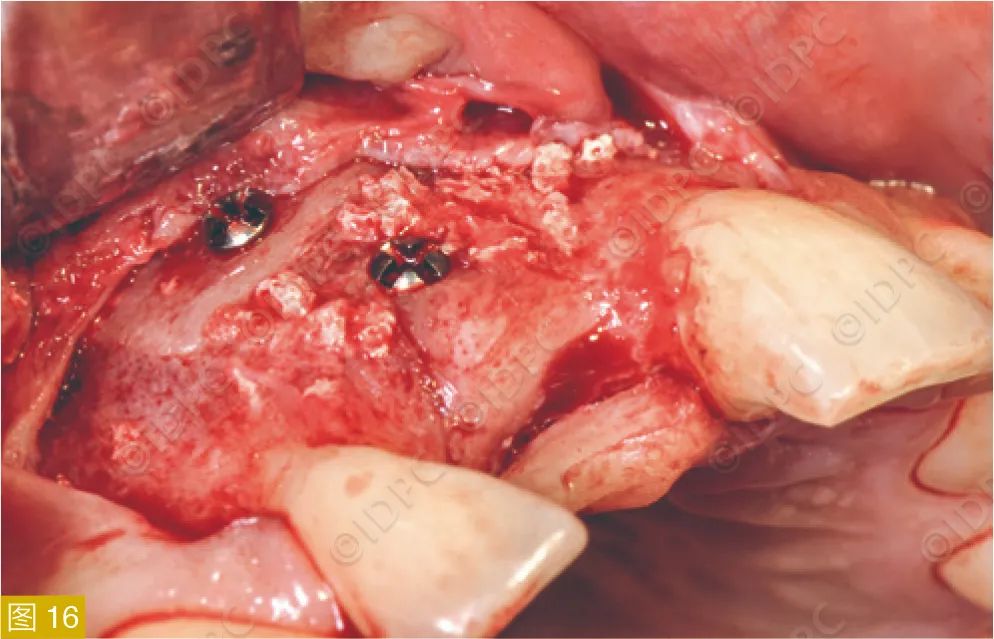
Four months post-augmentation, a surgical guide was fabricated using a vacuum-formed technique, positioning pre-fabricated sleeves based on the original location of tooth #11 (Figure 12). This allowed precise implant placement without considering the bone defect (Figures 13-14).



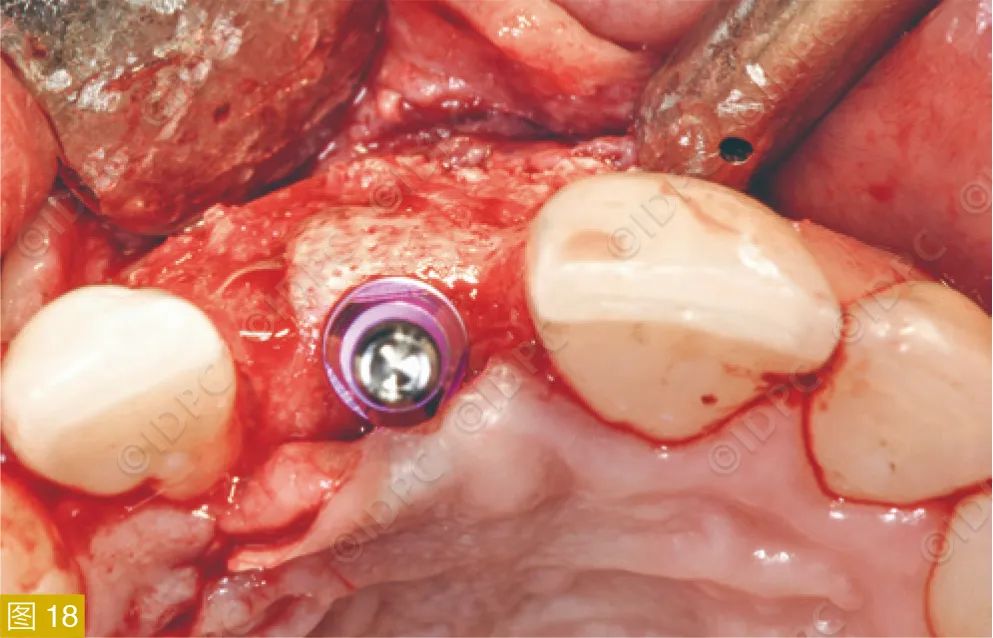
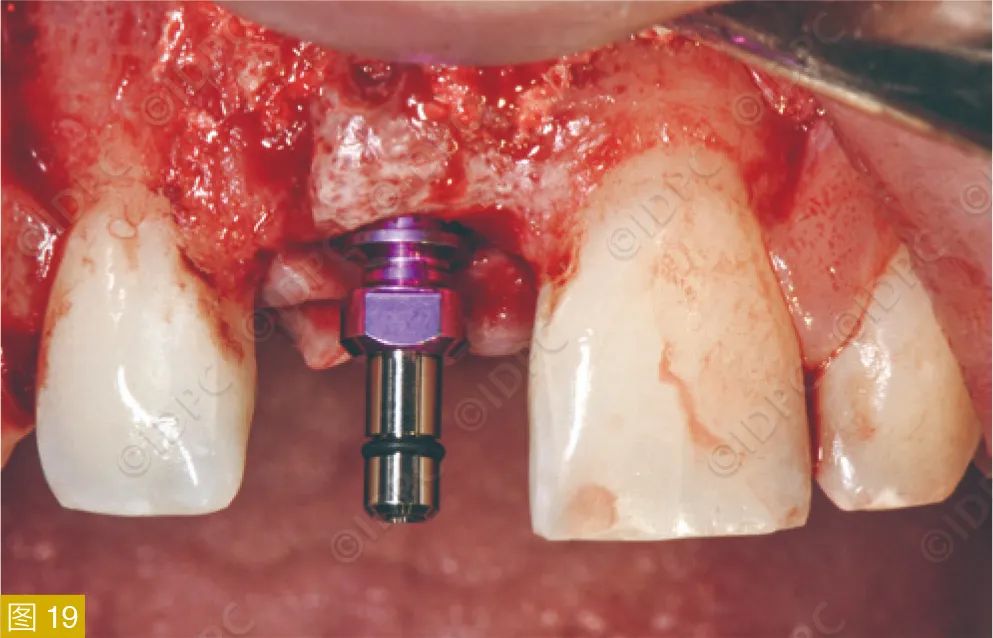
A mucoperiosteal flap was raised, revealing the well-integrated bone blocks and significant vertical and horizontal bone regeneration (Figure 16). After screw removal, the guide directed initial drilling (Figure 17), followed by sequential preparation and implant placement (Figure 18). The CAMLOG®
SCREW-LINE implant (4.3mm diameter, 13mm length) was surrounded by well-vascularized bone, ensuring stable placement (Figure 20).


**Soft Tissue Augmentation and Contouring**
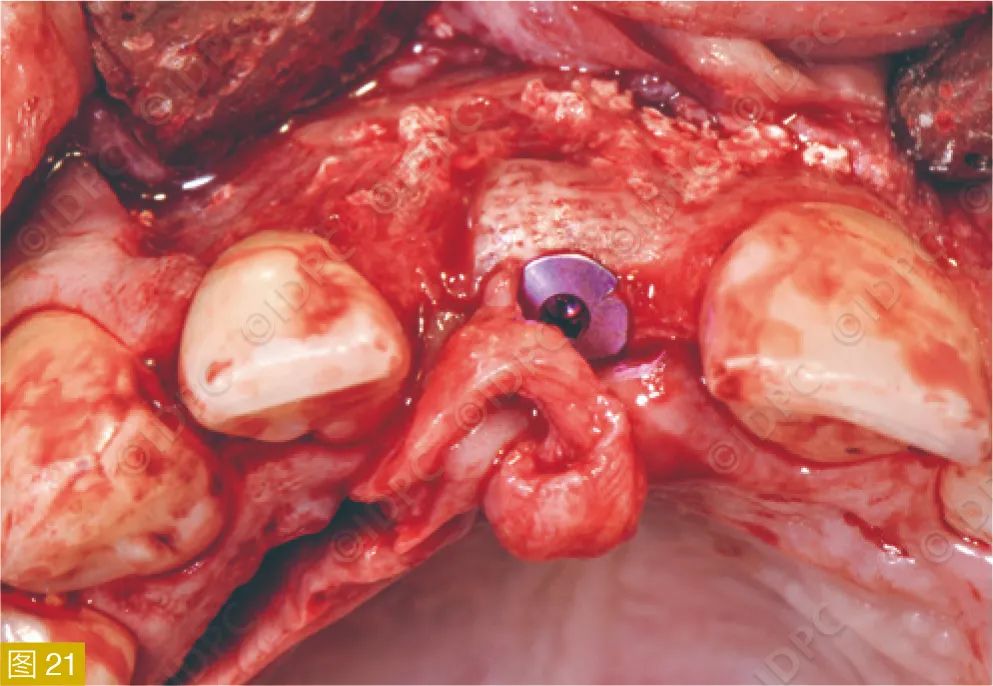
A pre-shaped palatal connective tissue graft was used for soft tissue augmentation immediately after implant placement. The graft was inserted through an anterior pedicle and sutured to the periosteum (Figures 21-23).


**Gingival Contouring**
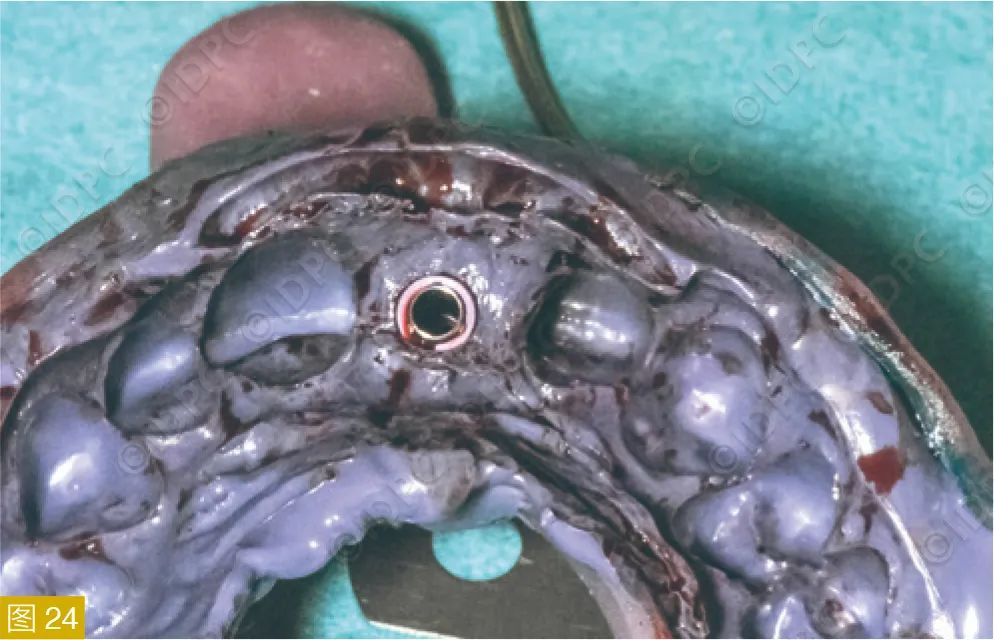
An individualized gingival former was fabricated based on an intraoperative impression taken with a custom tray (Figures 24-27). This former, exceeding the gingival margin by 2mm, was designed to replicate the anatomical crown dimensions, ensuring proper gingival contouring.



**Personalized Abutment and Implant-Supported Single Crown**
After removing the gingival former, an impression was taken using a custom impression post stabilized with low-viscosity resin to prevent gingival deformation (Figure 28). A personalized abutment was fabricated, addressing three tasks: custom color, gingival contouring, and crown margin positioning (Figure 29).




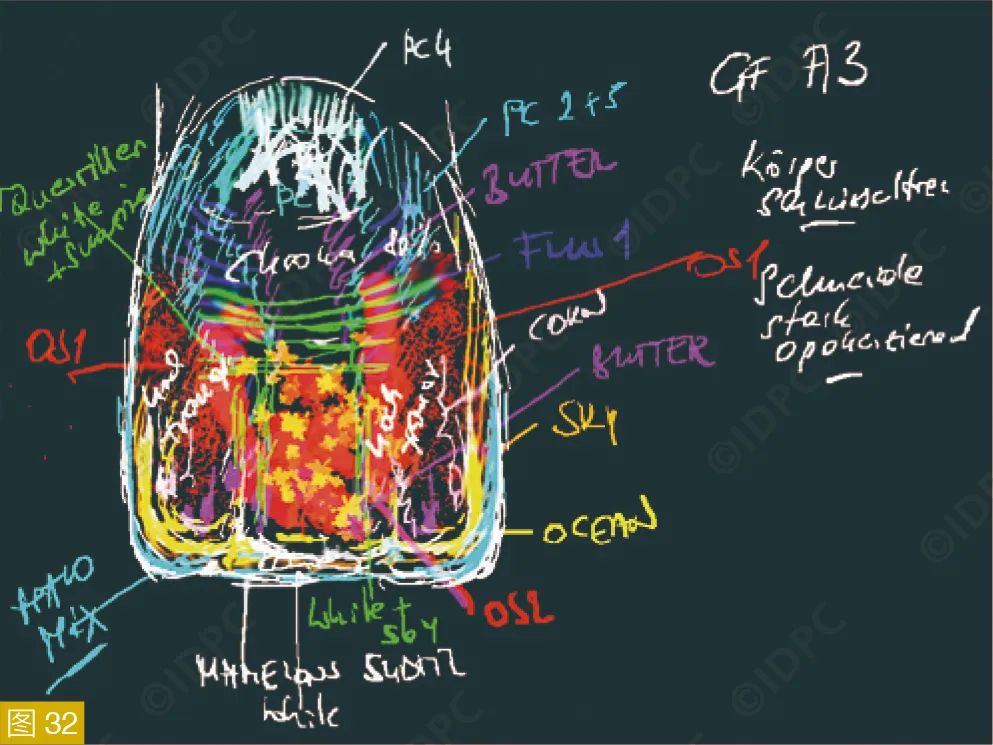
The fabricated crown was bonded to the abutment, and clinical photos were taken one month post-placement (Figure 33). A 15-month follow-up showed stable and satisfactory aesthetic and functional outcomes (Figure 34).


**Discussion/Summary**
This case illustrates the detailed process of aesthetic restoration of a missing anterior tooth. Extensive bone loss due to an enlarged cyst necessitated step-by-step hard and soft tissue regeneration. This treatment plan, extending over a year, involved standardized interdisciplinary collaboration, ensuring timely biological regeneration processes.
The key objectives of our treatment were:
– Comprehensive dental models and preoperative photographs (data backup)
– Minimally invasive tooth extraction
– Pathology-free surgical healing
– 3D hard tissue reconstruction
– Prosthetically guided implant placement (surgical guide)
– Adequate soft tissue reconstruction
– Personalized gingival contouring
– Custom abutment
– Detailed shade and characteristic determination
– Layered zirconia-veneered crown
This interdisciplinary effort, particularly with Dr. Otto Exenberger and dental technician Christian Koczy from Vienna, was crucial in achieving the successful prosthetic restoration for the patient.




Leave a Reply