Authors:
Dr. Karl-Ludwig Ackermann
Private Practice in Oral Surgery
Introduction
The concept of “No Implant Without Periodontics” (NIWOP) emphasizes the importance of integrating implant therapy with pre- and post-operative preventive measures, ensuring a consistent and fundamental approach. Diagnostics, prevention, and treatment must be tailored to each patient’s individual risks and susceptibilities. Key factors for long-term stable implant care include individualized risk management plans, patient education on oral hygiene and regular follow-up, and professional teeth cleaning at intervals tailored to the patient. Establishing and reinforcing good oral hygiene habits is best achieved by implementing NIWOP as a preventive workflow before planned restorative treatments, ensuring that implant therapies are conducted in an inflammation-free environment.
Background
Biofilm formation is a known cause of periodontal and peri-implant inflammation. In collaboration with Dr. Karl-Ludwig Ackermann and Prof. Anton Sculean, the Austrian family business W&H Dentalwerk Bürmoos introduced the NIWOP concept at the 2018 European Periodontology Congress in Amsterdam. This concept ensures stable periodontal conditions before implant treatment and maintains the stability of implant-supported restorations through continuous, personalized follow-up care.
While a minority of patients lose teeth due to trauma or other acute conditions, most gum inflammation results from chronic periodontal disease. Causes may include poor oral hygiene, genetic predisposition, or systemic diseases. In such adverse environments, should implant therapy be considered? Could it pave the way for peri-implantitis later on? (Figures 1 and 2).


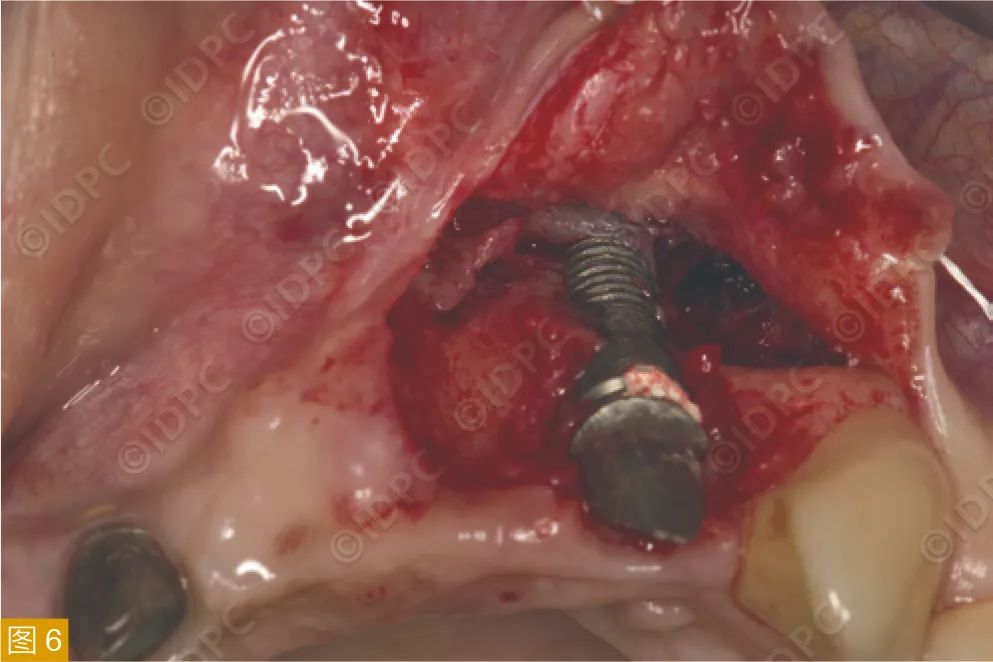
Nearly half of implant patients may develop mucositis, which can be controlled with current knowledge. However, over 20% of patients might progress to peri-implantitis (Figures 3-6). Despite effective methods and robust research, there is no standardized treatment for peri-implantitis. Therefore, its prevention is paramount. Expecting patients with historically poor oral hygiene to maintain ideal hygiene post-implantation is unrealistic. Similarly, patients with systemic diseases or reduced self-care ability may face post-implant inflammation risks. Hence, a comprehensive oral hygiene maintenance plan encompassing pre- and post-implant strategies is crucial.



Pre-Implant Maintenance
According to research, untreated periodontitis patients and those who received only initial treatment without supportive follow-up share similar high risks of developing peri-implantitis. NIWOP begins with pre-implant diagnostics, including PSI/PSR (Periodontal Screening Index/Periodontal Screening and Recording), BOP (Bleeding on Probing), and pocket depth measurements, along with noting systemic diseases posing specific risks. Diseases such as poorly controlled diabetes, rheumatoid arthritis, hypertension, cardiovascular diseases, or stroke should be considered. Many studies indicate periodontitis adversely affects these systemic conditions, although the exact pathological connections remain unclear, raising awareness in dental practices. Harmful habits like smoking should be addressed, providing positive interventions and effective support (motivational interviewing).
If a positive periodontal diagnosis is made, NIWOP protocols should start with initial periodontal treatment. Professional teeth cleaning, removal of supragingival and subgingival calculus, and biofilm, along with subgingival debridement using specialized sonic or ultrasonic instruments with periodontal tips, are essential. Additional periodontal or regenerative surgeries may be warranted. Patients must be educated on maintaining adequate oral hygiene at home, provided with appropriate maintenance tools, and trained in their correct use (if necessary, correcting brushing errors) (Figures 7-10).




At this stage, a follow-up schedule tailored to the patient’s individual circumstances and capabilities should be established to provide early intervention or professional support. Personalized professional periodontal follow-up care includes regular ultrasonic scaling, air polishing, or manual scaling to remove the continuously accumulating biofilm and plaque.
Treatment Process and Instruments
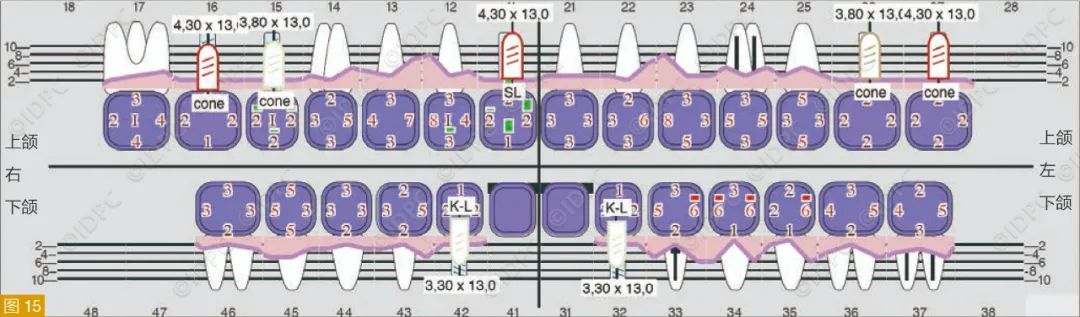
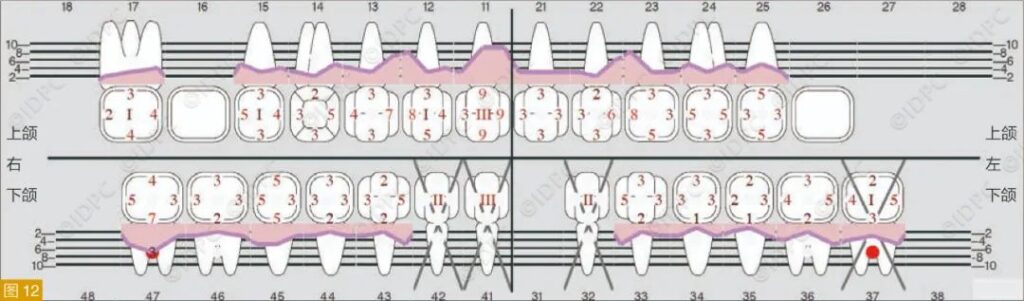
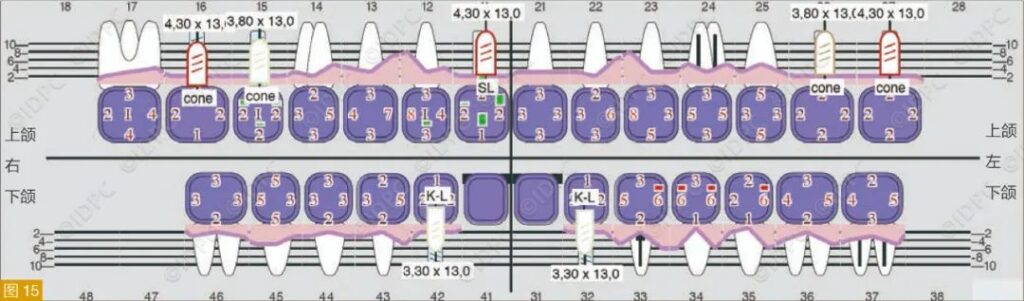
Implant therapy should only be planned once a stable periodontal condition is achieved (baseline state: Figures 11-13). Clear communication with the patient about the treatment process can motivate them to diligently maintain oral hygiene and comply with follow-up appointments. Minimally invasive implant treatments can be performed using ultrasonic bone surgery devices with tips specifically for bone and soft tissue handling or high-performance surgical motors with dedicated contra-angles for implant site preparation. The choice of implant system, restoration design, and cleaning methods should align with the patient’s individual risk factors. Special attention should be given to the implant-abutment connection area, ensuring minimal irritation, excellent biocompatibility, and mechanical stability. One-stage treatments (e.g., “one-time placement of permanent abutments”) ensure stable peri-implant conditions. Using ISQ (Implant Stability Quotient) measurements to assess initial stability allows for early or immediate loading post-implantation (Figures 14-16).




Post-Implant Follow-Up Care
As previously mentioned, experts recommend early intervention at the onset of mucositis to prevent the progression to peri-implantitis with accompanying bone loss. Patients must first be guided and trained on necessary home hygiene maintenance changes due to new restorations. Special emphasis should be placed on using interdental brushes from various angles to avoid injury and ensure thorough cleaning.
An individualized periodontal follow-up schedule of 2-4 times a year should continue post-implant treatment to monitor inflammatory changes early and ensure an inflammation-free state through regular professional teeth cleaning. Early signs of mucositis need immediate intervention through effective removal of supragingival and subgingival plaque to prevent further inflammation and peri-implantitis. Despite all preventive measures, if peri-implantitis occurs (e.g., due to poor patient oral hygiene), the use of appropriate ultrasonic instruments, Er:YAG laser assistance, antimicrobial photodynamic therapy (aPDT), air polishing, or local antibiotics are effective methods to control the inflammation (Figure 17). If non-invasive treatments are ineffective, surgical exposure and decontamination of the infected area are required, followed by soft and hard tissue augmentation if possible. Once reconstructed, preventive follow-ups need to resume, ideally on a more frequent basis.

Known and Must-Know Aspects
– Both periodontics and implants involve multidisciplinary dental collaboration.
– Epidemiologically, over 50% of young adults (35-44 years) and young elderly (65-74 years) suffer from moderate to severe periodontitis.
– The number of elderly is rapidly increasing, predicting a higher future demand for periodontal treatments despite a reduction in prevalence (around 2030).
– The primary demand for implants comes from elderly patients, with risks for diseases (mucositis or peri-implantitis) similarly increasing.
– Therefore, ensuring clean “healthy” teeth through pre-treatment and good maintenance is crucial for successful implant restorations, ensuring no complications.
– Knowledge of periodontal diseases and associated factors, along with a well-planned treatment timeline, are key to successful periodontal-implant restorative treatments.
Conclusion
No Implant Without Periodontics (NIWOP).




Leave a Reply